The Year of the Lung: outdoor air pollution and lung health
DOI: https://doi.org/10.4414/smw.2010.13129
Summary
With reference to the Year of the Lung, current knowledge of the respiratory effects of current ambient air pollution is reviewed. Acute respiratory effects are well established. Studies such as SAPALDIA and others now shed light on the long-term effects on chronic pathologies and on the health benefit of air quality improvements. The identification of those at highest risk and of local effects of not yet regulated traffic-related pollutants remains a research priority.
Introduction
The year 2010 has been proclaimed the international Year of the Lung to emphasise the importance of healthy lungs. The major threat to lung health is undoubtedly smoking. The emphasis of this short review will be a more ubiquitous and entirely involuntary threat to health, namely ambient air pollution, which is an established cause of morbidity and mortality [1]. Air pollution affects 100% of the population from cradle to grave. Large sections of European populations continue to live in areas with unhealthy air quality. For some pollutants and in some regions this situation is not improving and is even deteriorating. Moreover, changes in combustion and fuel technologies, industrial production, movement of goods and urban planning affect the constituents and thus possibly the toxicity of air pollution as well as the population’s exposure. Thus, while air quality improved in many areas in recent decades, the problem is by no means resolved and nor are all adverse effects well understood. The aim of this review is to provide a key selection of information around the respiratory health effects of ambient air pollution, with discussion of open questions and future prospects. While the evidence for adverse effects of air pollution beyond the involvement of the lung alone is steadily growing, embracing a wide range of cardiovascular outcomes including atherogenic effects, these are not the subject of this paper [2, 3]. A more detailed overview of the evidence has been published by the European Respiratory Society for the 2010 Year of the Lung and is freely available online in several languages [4]. This review lists only a selection of the key references, but more can be provided on request.
Air pollution composition and sources
Air pollution is a complex mixture of thousands of pollutants. This mixture may consist of solid and liquid particles suspended in air (particulate matter – PM), and different type of gases such as ozone (O3), nitrogen oxides (NO2 or NOx), volatile organic carbons (VOCs), and carbon monoxide (CO). While particles vary in number, size, shape, surface area and chemical composition, both particles and gases may vary in solubility and toxicity. The most important processes causing air pollution relate to the combustion of fossil fuels used in cars and trucks, aircraft, marine vessels or other engines, as well as in industry, power plants, or household heating systems. Due to the close proximity between people and emissions, transport-related activities, in particular involving cars and trucks, are an important source of air pollutants. Traditionally, health studies have used markers of air pollution to study its effects, e.g. the mass of size specific PM fractions – such as PM10 or PM2.5 – NO2, or distance to main roads.
Air pollutants orchestrate pathophysiologies
While experimental studies confirm a range of effects related to single pollutants, it should be emphasised that the effects of ambient air pollution cannot be attributed to one single pollutant in the mixture. In contrast – as in case of tobacco smoke – many pollutants act together in a series of partly interrelated mechanisms, which result in the observed associations between current levels of air pollution and a range of health outcomes. Oxidative stress and both local and systemic inflammation are suggested as main mechanisms following the inhalation of these pollutants [5]. A first step may be the release of reactive oxygen species of lung cells (e.g. through contact with inhaled particles where toxic substances such as metals are adsorbed). Particulate matter of various sizes, as well as highly oxidative gases (e.g. O3 or NOx) have been shown to induce local pulmonary reactions related to oxidative stress [6, 7]. Both local and systemic inflammatory reactions, mediated through cytokines and chemokines, have been described in experimental studies in cellular systems, animals, and in chamber studies with human subjects [8].
Respiratory health effects
The respiratory tract is the portal of entry of air pollutants, and thus the lung is the first affected organ. The range of respiratory diseases due to air pollution exposure is wide. Studies on the health effects of air pollution distinguish between acute and chronic effects. The acute effects of pollution may be expressed within hours or days of exposure, but other health effects of air pollution result from long-term exposures leading to chronic pathologies. While the acute and chronic effects of air pollution are partly interrelated, the distinction is important when planning and interpreting epidemiological studies and for policymaking.
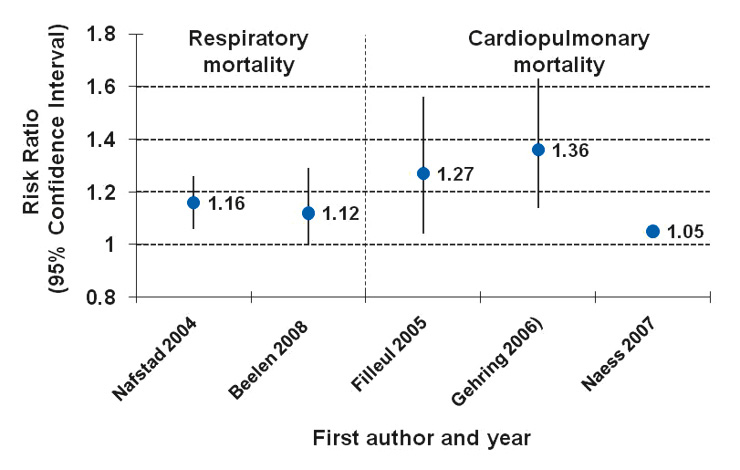
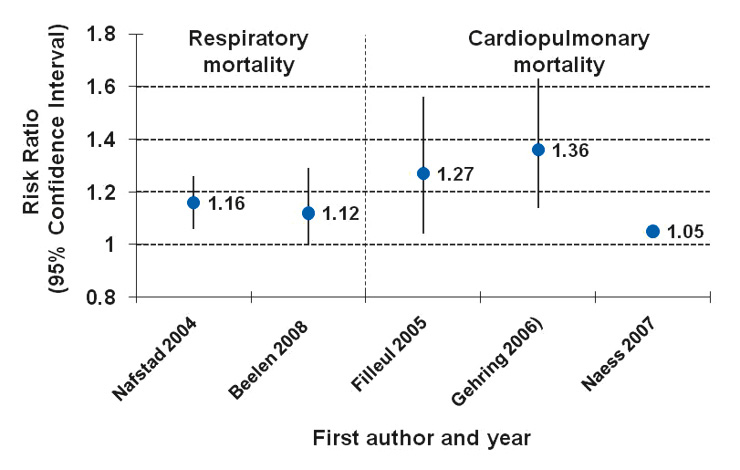
Figure 1
Relative risks (RR) for respiratory [44, 45] or cardiopulmonary mortality [46–48] with 95% confidence intervals (CI) from European cohort studies on air pollution expressed per 10 µg × m–3 NO2 or NOx. (No CI available for cardiopulmonary estimate in [48].)
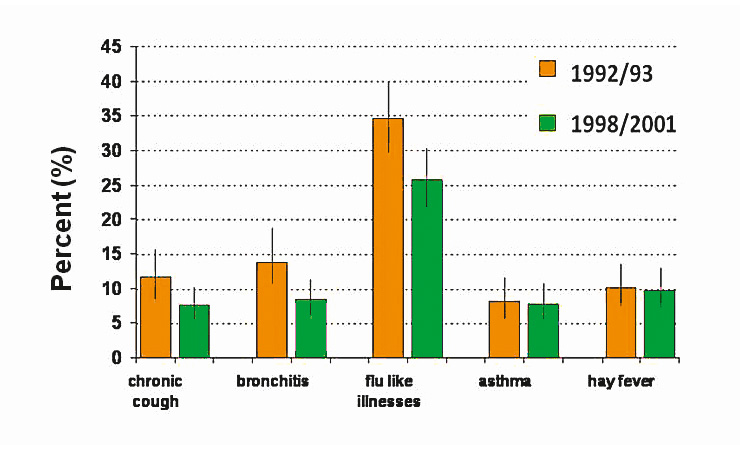
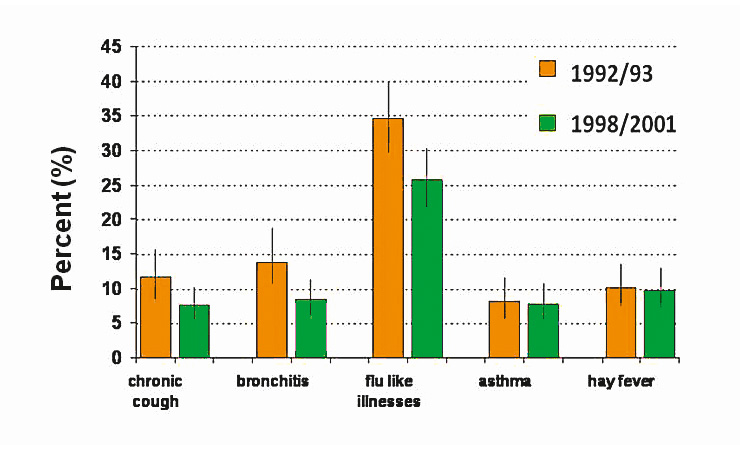
Figure 2
Prevalence of respiratory illnesses in Swiss schoolchildren after the improvement of air quality in the nineties, SCARPOL Study [17].
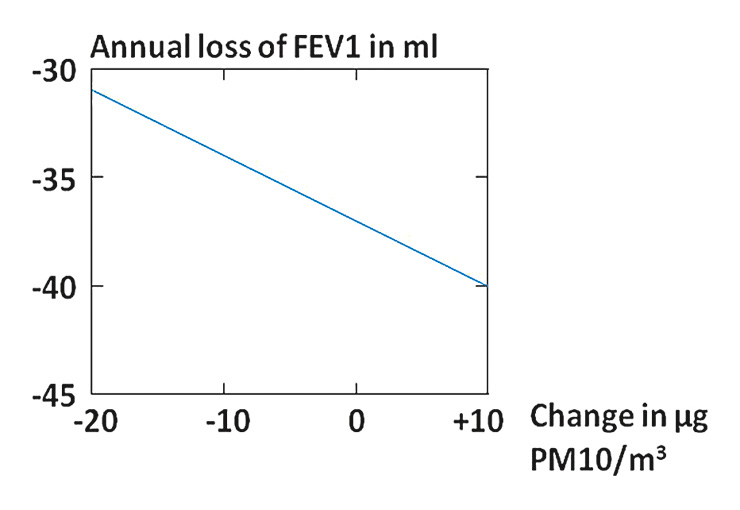
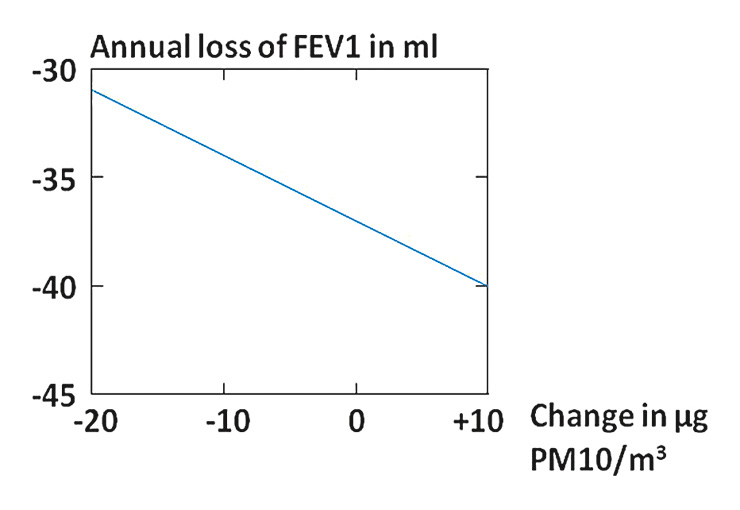
Figure 3
Decrease of PM10 from 1991 to 2002 and age-related loss of lung function in Swiss adults in the SAPALDIA study [13]. An increase in air quality of 10 µg PM10 × m–3 diminished the age-related loss of FEV1 by 3.1 ml annually.
Short-term respiratory effects of air pollution
Daily mortality
A large number of epidemiological studies have shown that the daily number of deaths, mainly from cardiovascular and respiratory diseases, follows the daily fluctuation of air pollution [9]. APHEA, the seminal European multicity time series analyses carried out in 29 study centres including three Swiss cities, found an increase in deaths from illness of 0.6% per 10 µg × m–3 increase in PM10 concentration, and data from hundreds of cities around the world observed similar results. Studies on short-term mortality showed that in general the air pollution-related relative risk is higher for respiratory outcomes. However, as more people die from cardiovascular diseases, the number of cardiovascular deaths related to air pollution is as large or larger than the number of respiratory deaths attributable to air pollution.
Daily respiratory disease exacerbations
The daily variation in disease burden due to urban pollution is also shown by increases in the numbers of emergency visits and hospital admissions due to respiratory diseases, including asthma. APHEA found increases of 1.2% for asthma in children; 1.1% for asthma in adults aged up to 64 years; and 0.9% for all respiratory diseases (including COPD, asthma and other respiratory diseases) in the elderly per 10 µg × m–3 increase in PM10 concentration.
Patients with asthma, especially children without anti-inflammatory or bronchodilator therapy, suffer more on or after days with higher pollution levels. Panel studies on asthmatics employing rigorous exposure assignment methods have found increased wheezing, cough and attacks of breathlessness, accompanied by poorer lung function and need for additional medication, associated with daily variations in PM, NO2 and/or O3.
Long-term consequences of air pollution
Long-term or lifetime exposure to ambient pollutants may also contribute to pathologies that ultimately result in chronic respiratory diseases. Investigation of these effects usually requires large studies and, ideally, follow-up investigations over many years, and thus fewer studies have investigated these types of effect. Indeed the Swiss SAPALDIA cohort study – now in its 20th year since inception – has been one of the very few epidemiological studies initiated from the very beginning to investigate the long-term effects of ambient air pollution. In the past 10 years SAPALDIA and several other studies have also confirmed adverse effects of ambient air pollution that are of chronic nature [10–13].
Mortality and life expectancy
Studies conducted in Europe, the USA and Canada confirm that the overall effects of pollution on mortality are far larger than the fraction attributed to acute exposures. Respiratory diseases are in general less often the cause of death than cardiovascular diseases. Therefore, the two are often combined in the category of cardiopulmonary mortality. Cardiopulmonary mortality was associated with long-term differences in particles and sulphate concentrations between cities in the Harvard Six Cities Study and in the American Cancer Society (ACS) study [14, 15]. Comparison of community-level concentrations of fine particles with death rates among more than 500 000 participants in the ACS study showed a 6% increase in cardiopulmonary deaths 16 years later per 10 µg × m–3 of PM2.5. In a reanalysis of
18 years of ACS follow-up from the Los Angeles area, modelled PM2.5 concentrations were assigned to each residence. This improved exposure assignment resulted in larger estimates. Cardiopulmonary mortality increased by 20% per 10 µg × m–3 contrast in PM2.5 [16].
Cohort studies in Europe have been able to confirm the relationship between cardiopulmonary death risk and pollution (fig. 1). Three European studies were able to analyse the data for respiratory and cardiovascular mortality separately. The results showed that urban air pollution, assessed individually for all participants by modelling traffic emissions of NOx, was associated with overall mortality, mortality from ischaemic heart diseases, respiratory mortality, lung cancer mortality and weakly also with cerebrovascular mortality. A Dutch cohort study with exposure data over 20 years observed weak associations of traffic density on the nearest main road with cardiopulmonary death. Respiratory deaths were related to NO2, black smoke, traffic density within a radius of 100 m, and living near a main street.
Respiratory disease incidence in children
Children are more active and engage in more outdoor activities. They breathe faster and their metabolic rate is higher than in adults. Children’s immune systems are not fully developed, and thus the incidence of respiratory infections is high. The lung is still growing and any deficit in growth will be relevant throughout the child’s life. Moreover, possible confounding or modifying factors, such as active smoking, occupational exposure to dust and smoke or medical treatments for disease, are largely absent, making the interpretation of epidemiological results more straightforward. Of particular interest and relevance are investigations of lung function development in children and the incidence of asthma, the main chronic disease in children.
Symptoms: Several cross-sectional studies from Germany, Switzerland, France and the USA found as early as the 1980s, and have confirmed in very recent studies, that school-age or preschool children in communities exposed to higher levels of dust, SO2 and NO2 suffer more from cough and acute bronchitis than children in less polluted regions. With improving air quality the prevalence of some respiratory symptoms in schoolchildren decreases (fig. 2).
Lung function (spirometry): More recently, many cross-sectional studies have reported lower lung volumes in children living in more polluted areas. Of outstanding importance is the largest and most detailed long-term study ever done on air pollution and lung development in children, namely the USC Children’s Health Study. Several cohorts recruited during elementary or middle school and followed up into adulthood confirm that ambient air pollution jeopardises the development of children’s lungs, resulting in lower lung function volumes and flows at age 18 [18]. The finding of a unique Swiss birth cohort study indeed indicated that exposure to ambient air pollution during pregnancy leads to possibly prime adverse developments of the lung [19].
Childhood asthma: While exacerbations of asthma clearly correlate with air quality, geographical comparisons of the prevalence of asthma or allergies do not follow gradients in urban background levels of pollutants. Novel approaches now integrate local measurements of traffic-related pollutants, geographic information systems, land-use data and spatial modelling techniques to characterise the local intra-community distribution of traffic-related pollutants. People living on busy roads experience several-fold higher exposures to traffic-related primary pollutants than people living some 50–100 m away. Epidemiological studies investigating the prevalence of childhood asthma as a function of proximity to traffic strongly suggested that living close to a busy road increases the risk of developing childhood asthma, even when confounding factors are taken into account. Despite rather different urban structures, traffic patterns and car fleets, this has now been confirmed in seminal cohort studies both in the US (e.g. the USC Children’s Health Study) and Europe. Most importantly, a European birth cohort, with children now followed up to eight years of age, confirmed a higher incidence of asthma due to ambient air pollution [20]. The USC study is highly suggestive of an interaction between genetic factors and exposure to traffic-related pollutants [21].
The contrasting lack of association between asthma onset and urban background pollution, and strong associations between proximity to traffic arteries and asthma incidence – allowing for socio-economic differences – suggest a relevant asthmogenic role of those pollutants occurring at very high concentrations along street corridors (e.g. ultrafine particles, black carbon, particle bound metals, aldehydes). Urban planning decisions may therefore have major public health implications. Study results place diesel cars, trucks, and buses emitting particularly high concentrations of soot and large numbers of very toxic substances loaded on particles from exhaust, abrasion, and suspension at the centre of the policy debate. This may become of particular concern in emerging megacities in the South (e.g. Africa, Asia), where millions live and work in proximity to ever-increasing flows of vehicles with very poor regulations on exhaust control, maintenance and fuel quality [22].
Chronic respiratory disease in adults
The most important risk factor for chronic respiratory diseases in adults is smoking, and the health effects of smoking and ambient air pollution appear largely to overlap. Studies evaluating the impact of outdoor air pollution on diseases such as chronic obstructive pulmonary diseases (COPD) and asthma in adults need to take into account the correlation of these factors, in addition to individual traits such as age, sex and genetic factors. Studies with results based on never-smokers are particularly valuable.
Symptoms: Chronic cough and phlegm, as well as lung function decrements, have been associated with long-term ambient PM exposure in several repeated cross-sectional studies in the USA and
Europe. Interestingly, some of these studies have shown that respiratory symptoms are more prevalent among participants living in proximity to main streets, independently of background pollutant concentrations.
Lung function and COPD: Many studies reported cross-sectional associations between lung function and air pollution, although some of these results are partly inconsistent, possibly due to methodological causes [23]. Most importantly, in the Swiss SAPALDIA study reduction in exposure to pollutants attenuated the age-related decline in lung function (fig. 3) [13].
While a few studies support the notion that air pollution may also contribute to the development of COPD, further investigations are needed [24], major difficulties of this assessment relating to general challenges and uncertainties in COPD research. While air pollution is clearly associated with reduced lung function development in children (see above), how low lung function in early life relates to the development of COPD is poorly understood. Moreover, air pollution triggers respiratory symptoms and aggravates infections, but it is not known how these findings relate to the development of COPD; cohort studies confirm that those with chronic symptoms and repeated infections are at higher risk of developing COPD. Last but not least, it is not well established whether COPD in non-smokers and smokers can be considered the same phenotype, and the difficulty of properly defining COPD both clinically and epidemiologically is a challenge for air pollution and any other aetiologic research as well [6].
Adult asthma incidence: As in children, asthma in adults is not correlated with urban background levelsof pollution such as PM2.5. However, the few studies investigating the contribution of local traffic-related air pollution to asthma onset in adults have produced similar findings to those looking at childhood asthma incidence [11]. More research is needed to clarify these results and the interaction with atopy, genetics and other host factors [25].
Lung cancer: Lung cancer is a relatively rare disease in non-smokers, with a long latency period. The time from diagnosis to death is often short and treatment is of limited success. To look at lung cancer in population-based studies, the population sample has to be large and the follow-up time long. Therefore, despite the coherence of experimental information, occupational studies and many results in population studies, not all long-term epidemiological studies have shown a link between ambient air pollution and lung cancer mortality. In the American Cancer Society cohort study, the incidence of lung cancer increased by 8% per 10 µg × m–3 increase in PM2.5 levels measured as a between-city difference; in a Danish cohort study, lung cancer incidence increased by 3.7% per 10 µg × m–3 increase in NOx used as a marker of exposure to traffic-related pollutants. Most importantly, particles – in particular those from diesel engines – are loaded with carcinogens. The Californian EPA lists diesel as an established carcinogen [26–28].
The large European research consortium ESCAPE will add to the evidence of long-term
effects of air pollution on chronic diseases, including a range of respiratory ailments such as asthma, COPD and bronchitis, as well as the development of lung function (http://www.escapeproject.eu).
Rigorous and standardised assessment of the European’s exposure to traffic-related pollution will highlight future policy needs tackling air quality along busy roads and highways.
The importance of susceptibilities
To understand and interpret the respiratory health effects observed, it is crucial to acknowledge the relevance of susceptibility (or protective) factors that modulate people’s reaction in the light of exposure to ambient pollutants. The identification of susceptibility factors is a subject of intense research (table 1). Given the relevance of the above-mentioned pathophysiological mechanisms, it is not surprising that an increasing number of studies report stronger effects of air pollutants in subjects with limited capacities to defend against oxidative stress and balance inflammatory responses. Such modulating factors may relate to sex, age, underlying diseases, pro- and anti-oxidant intake, and a range of genetic characteristics. For example, several investigations showed significantly increased morbidity and mortality rates in individuals with COPD following exposure to air pollution [29, 30]. As an example of concurrent risk relationships, a controlled trial in Mexican children confirmed not only the association between ozone and respiratory health, but revealed interactions related to oxidative stress pathways: children under anti-oxidant treatment where far less affected by ozone than the placebo groups, and children with functional variants of the GSTM gene were protected against the adverse respiratory effects of ozone as well [31].
|
Table 1Susceptibility factors identified in relation to childhood asthma as compiled in [43]. |
|
Susceptibility factor
|
Description
|
| Prenatal exposure to air pollution |
Increased risk for reduced lung function and asthma onset in children |
| Individual host characteristics(atopy, sex, nutritional status) |
Greater susceptibility to air pollution-mediated asthma exacerbations |
| Chronic stress |
Modify asthma exacerbations associated with traffic-related air pollution exposure |
| Gene-environment interactions |
Polymorphisms in genes involved in metabolism of oxidant species, airway inflammation, and innate immunity modify response to air pollution exposures |
Relevance and outlook
Just as medicine should be evidence-based, public health action and policy must be grounded in science [32]. Several “semi-experimental” studies have been conducted in recent years, reporting on the impact – or “accountability” – of air quality improvements in health, represented by a reduction of symptoms and improvement in life expectancy [33–37]. An additional concrete example, as mentioned earlier, are the concerted policies implemented in Switzerland and neighbouring countries in the 1990s which resulted in a decrease in air pollution and a range of health improvements [13, 38, 39]. Repeated cross-sectional investigations in school classes observed a decrease in irritative symptoms and respiratory disease in children (fig. 2). This change correlated with a decline in PM levels. Similarly, the Swiss cohort study SAPALDIA followed lung function decline among adults during the same time span. Age-related lung function decline was associated with air quality; in particular, the 11-year decrease in individually estimated home outdoor PM10 levels was associated with an attenuated decline in lung function (fig. 3). Air quality improvements also had a beneficial effect on respiratory symptoms: a mean decline of PM10 of 6 µg × m–3 coincided with 259 fewer subjects with regular cough, 179 fewer subjects with chronic cough or phlegm and 137 fewer subjects with wheezing with breathlessness per 10 000 adults. Moreover, a decline in new onset of asthma in adults, indicated by chronic cough, was associated with the change in pollution.
Despite many open questions, there is sufficient evidence to press for sustained improvements in air quality all over the world. For this current scientific knowledge must reach policy makers in a comprehensible way. As with tobacco smoke, the voice of health professionals is instrumental in shaping the opinions of the public and policy makers. Swiss and European research findings make a strong case for sustained improvements in air quality to support public health. In fact, the early trinational European health impact assessment of air pollution [40] emphasised what several local and Trans-European analyses have confirmed since: the public health impact of air pollution is very substantial, and thus the benefits of a reduction in air pollution will be large both in terms of cost-relevant morbidities and life expectancy. These risk assessments are inherently incomplete, since newly emerging effects that may be attributable to air pollution are not considered at all. For example, methodological work on risk assessment has shown that not taking into account the impact of air pollution on the new development of asthma in children (i.e. asthma incidence) can grossly underestimate the impact of air pollution on asthma-related health problems [41, 42]. If a child develops asthma due to traffic-related air pollution, it is indeed appropriate to attribute the entire future asthma career, for example any exacerbation event, to this environmental cause – traffic air pollution – no matter whether some asthma crisis may be caused by air pollution generated by other sources or any other effect (i.e. pollen exposure). However, while this is conceptually sound, one needs to emphasise that it is not known at all whether removing air pollution would prevent the development of asthma in such cases altogether, or only postpone the onset of asthma due to some other competing risks.
With the improvement of air pollution exposure assessment technologies, other health outcomes are becoming of increasing interest due to plausible pathways connecting the lung with other organs and systemic effects. A better understanding of specific effects of the various sources and components of air pollution, including nano-size-combustion-related pollutants [6, 7], will enhance our understanding of the total effect and improve the regulatory framework for the ultimate protection of public health.
Correspondence to:
Prof. Nino Künzli, MD PhD
Swiss Tropical and Public Health Institute
Socinstrasse 57
CH-4051 Basel
Switzerland
Nino.Kuenzli@unibas.ch
References
1 WHO, World Health Organization. Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. global update 2005. WHO/SDE/PHE/OEH/06.02. 2005.
2 Brook RD, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78.
3 Kunzli N, Tager IB. Air pollution: from lung to heart. Swiss Med Wkly. 2005;135(47–48):697–702.
4 Kunzli N, Perez L, Rapp R. Air quality and health. European Respiratory Society. Switzerland. Available at http://www.ersnet.org ., 2010.
5 Romieu I, et al. The effect of supplementation with omega-3 polyunsaturated fatty acids on markers of oxidative stress in elderly exposed to PM(2.5). Environ Health Perspect. 2008;116(9):1237–42.
6 Jochmann A, et al. General practitioner’s adherence to the COPD GOLD guidelines: baseline data of the Swiss COPD Cohort Study. . Swiss Med Wkly. [Epub ahead of print], 2010.
7 Muhlfeld C, Gehr P, Rothen-Rutishauser B: Translocation and cellular entering mechanisms of nanoparticles in the respiratory tract. Swiss Med Wkly. 2008;138(27–28):387–91.
8 Pope CA, 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc. 2006;56(6):709–42.
9 Samoli E, et al. Acute effects of ambient particulate matter on mortality in Europe and North America: results from the APHENA study. Environ Health Perspect. 2008;116(11):1480–6.
10 Imboden M, et al. Decreased PM10 exposure attenuates age-related lung function decline: genetic variants in p53, p21, and CCND1 modify this effect. Environ Health Perspect. 2009;117(9):1420–7.
11 Kunzli N, et al. Traffic-related air pollution correlates with adult-onset asthma among never-smokers. Thorax. 2009;64(8):664–70.
12 Felber Dietrich D, et al. Differences in heart rate variability associated with long-term exposure to NO2. Environ Health Perspect. 2008;116(10):1357–61.
13 Downs SH, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med. 2007;357(23):2338–47.
14 Dockery DW, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329(24):1753–9.
15 Pope A, Thun M, Namboodiri M. Particulate air pollution as a predictor of mortality in a prospective study of U.S adults. Am J Respir Crit Care Med. 1995;151:669–74.
16 Jerrett M, et al., Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology. 2005;16(6):727–36.
17 Bayer-Oglesby L, et al. Decline of ambient air pollution levels and improved respiratory health in Swiss children. Environ Health Perspect. 2005;113(11):1632–7.
18 Gauderman WJ, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004;351(11):1057–67.
19 Latzin P, et al. Air pollution during pregnancy and lung function in newborns: a birth cohort study. Eur Respir J. 2009;33(3):594–603.
20 Gehring U, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010;181(6):596–603.
21 Gilliland FD. Outdoor air pollution, genetic susceptibility, and asthma management: opportunities for intervention to reduce the burden of asthma. Pediatrics. 2009;123(Suppl 3):S168–73.
22 Dionisio KL. et al. Within-neighborhood patterns and sources of particle pollution: mobile monitoring and geographic information system analysis in four communities in Accra, Ghana. Environ Health Perspect. 2010;118(5):607–13.
23 Götschi T, et al. Long term effects of ambient air pollution on lung function – a review. Epidemiology. 2008;19:690–701.
24 Eisner MD, et al. Novel risk factors and the global burden of COPD: An official ATS public policy statement. I. American Journal of Respiratory and Critical Care Medicine 2010. In press.
25 Castro-Giner F, et al. Traffic-related air pollution, oxidative stress genes, and asthma (ECHRS). Environ Health Perspect, 2009;117(12):1919–24.
26 Nafstad P, et al. Lung cancer and air pollution: a 27 year follow up of 16 209 Norwegian men. Thorax. 2003;58(12):1071–6.
27 Raaschou-Nielsen O, et al. Air pollution from traffic and risk for lung cancer in three Danish cohorts. Cancer Epidemiol Biomarkers Prev. 2010;19(5):1284–91.
28 Pope, C.A., 3rd, et al., Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002;287(9):1132–41.
29 Sint T, Donohue JF, Ghio AJ. Ambient air pollution particles and the acute exacerbation of chronic obstructive pulmonary disease. Inhal Toxicol. 2008;20(1):25–9.
30 Zanobetti A, Bind MA, Schwartz J. Particulate air pollution and survival in a COPD cohort. Environ Health. 2008; 7:48.
31 Romieu I, Moreno-Macias H, London SJ. Gene by environment interaction and ambient air pollution. Proc Am Thorac Soc. 2010;7(2):116–22.
32 Kunzli N, Perez L. Evidence based public health – the example of air pollution. Swiss Med Wkly. 2009;139(17–18):242–50.
33 van Erp A, Cohen A. HEI’s Research Program on the Impact of Actions to Improve Air Quality: Interim Evaluation and Future Directions. Communication 14. Health Effects Institute, Boston, MA. 2009.
34 van Erp AM, et al. Evaluating the effectiveness of air quality interventions. J Toxicol Environ Health A. 2008. 71(9–10):583–7.
35 Pope CA, 3rd, Ezzati M, Dockery DW: Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009;360(4):376–86.
36 Clancy L, et al. Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet. 2002;360(9341):1210–4.
37 Heinrich J, et al. Improved air quality in reunified Germany and decreases in respiratory symptoms. Epidemiology. 2002;13(4):394–401.
38 Schindler C, et al. Improvements in PM10 exposure and reduced rates of respiratory symptoms in a cohort of Swiss adults (SAPALDIA). Am J Respir Crit Care Med. 2009;179(7):579–87.
39 Bayer-Oglesby LGL,Gassner M, Takken-Sahli K, Sennhauser FH, Neu U, et al. Decline of ambient air pollution levels and improved respiratory health in Swiss children. Env Health Perspect. 2005;113(11):1632–7.
40 Künzli N, et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet. 2000;356(9232):795–801.
41 Perez L, et al. Global goods movement and the local burden of childhood asthma in southern California. Am J Public Health. 2009;99(Suppl 3):S622–8.
42 Kunzli, N, et al. An attributable risk model for exposures assumed to cause both chronic disease and its exacerbations. Epidemiology. 2008;19(2):179–85.
43 Patel MM, Miller RL. Air pollution and childhood asthma: recent advances and future directions. Curr Opin Pediatr. 2009;21(2):235–42.
44 Nafstad P, et al. Urban air pollution and mortality in a cohort of Norwegian men. Environ Health Perspect. 2004; 112(5):610–5.
45 Beelen R, et al. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ Health Perspect. 2008;116(2):196–202.
46 Filleul L, et al. Twenty five year mortality and air pollution: results from the French PAARC survey. Occup Environ Med. 2005;62(7):453–60.
47 Gehring U, et al. Long-term exposure to ambient air pollution and cardiopulmonary mortality in women. Epidemiology. 2006;17(5):545–51.
48 Naess O, et al. Relation between concentration of air pollution and cause-specific mortality: four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo, Norway. Am J Epidemiol. 2007;165(4):435–43.