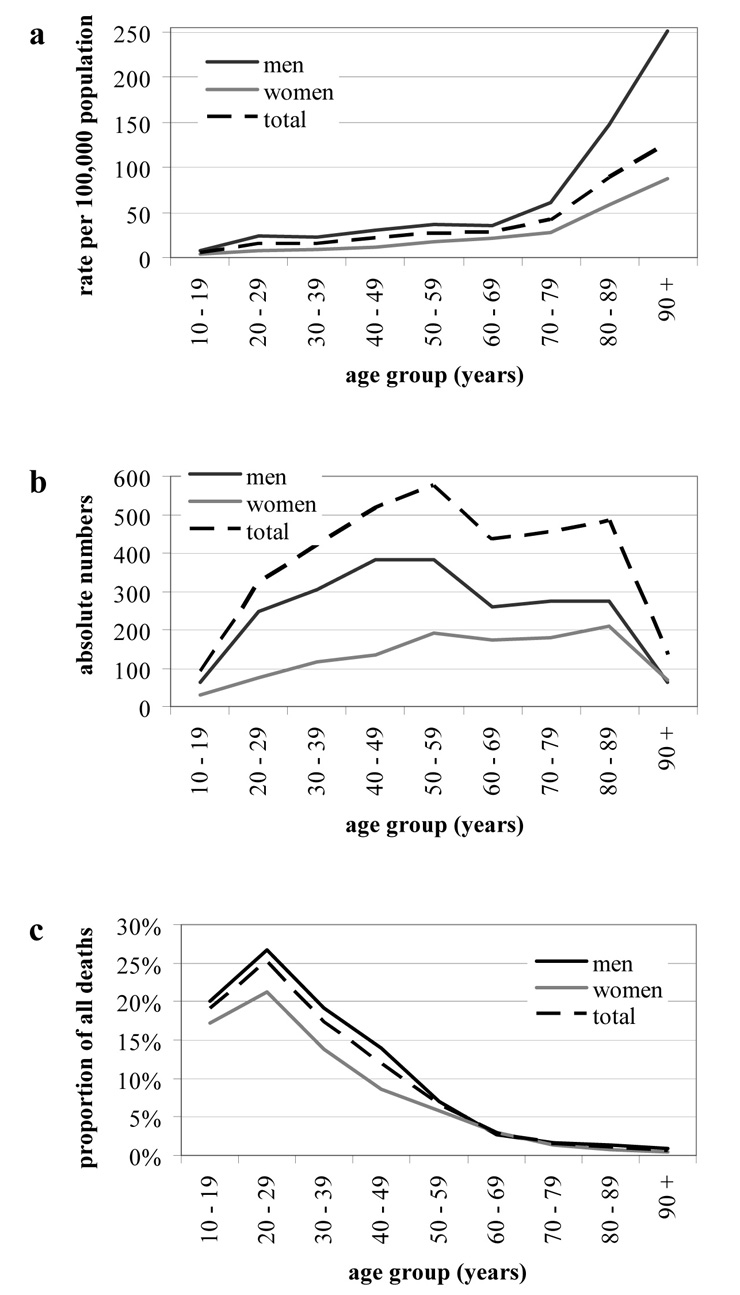
Figure 1
Mean suicide rates per year (a), suicide counts (b) and suicide proportions of all deaths (c) by age group and sex, in the Canton of Zurich, 1995–2007.
DOI: https://doi.org/10.4414/smw.2010.13102
Suicides are often investigated on a national level, but within Switzerland there are considerable regional differences, for example between the cantons (which are the member states of the federal state of Switzerland). According to a recent report by the Swiss Health Observatory, the suicide rate in the Canton of Zurich is 21.7 per 100'000 people (average over seven years from 2000 to 2006 [1]), and Zurich ranks fourth highest among the cantons. In that study [1], highest suicide rates were found in the Canton of Schaffhausen (25.9 per 100'000 population), whilst lowest rates were found in the Canton of Ticino (11.5 per 100'000 population).
A number of sociodemographic factors, such as sex, age, marital status or religion, are correlated with suicide rates. In Western countries, men commit suicide more frequently than women with male to female ratios between 2:1 and 4:1 [2]. The reasons for the male predominance of completed suicide seem complex. It has been proposed that men use more immediately lethal methods of suicide [3] and avoid acknowledging a need for help [2]. Suicide rates generally increase with age [2, 4–6], but this may be different for men and women [2,4], or rural and urban populations [5]. Additionally some countries in Central and South America or Eastern Europe, in contrast, show no significant increase in suicide rates with increasing age [7].
Marital status and religious affiliation can be regarded as forms of social integration that were proposed to correlate with lower suicide rates as suggested by Durkheim [8]. Also more recent studies confirm that being married is a protective factor [6] and can even buffer socio-economic inequalities with respect to suicide [9]. Within Switzerland, cantons with a higher percentage of Catholics generally have lower suicide rates [10].
Other factors associated with a higher risk for suicide are mental illnesses, such as depression or alcoholism [11,12], the presence of a possibly incurable somatic disorder, such as cancer [13, 14], or socioeconomic factors, such as lower levels of education and unemployment [10, 15, 16].
Suicide methods chosen depend on availability, but also correlate with sex, age and culture [17]. For instance, firearm suicide rates are higher where firearms are commonly stored in private households [18–20]. Swiss density of household firearms is comparatively high with an estimated 2.5 million firearms stored in private households (partly due to our military service customs). Among men, Switzerland has a higher proportion of firearm suicides compared to other countries [21, 22].
Using data from the Swiss statistics on causes of death, we investigated a number of statistically documented sociodemographic factors and variables pertaining to suicide methods and their impact on suicide rates in the Canton of Zurich. This study showed that suicide rates vary also among different regions (i.e. types of municipalities) within the Canton of Zurich. Such a detailed analysis appeared to be absent from suicide analysis in the Canton of Zurich so far. To discriminate the influence of various variables, a statistical model (logit) was used. Since this was a retrospective study, only those variables present in the data set could be explored, whereas a prospective study would allow the inclusion of other variables of interest. Thus, declared suicide motives, suicide attempts, the impact of assisted suicide or correlations with communally varying suicide prevention programmes were not examined in this study.
All data were obtained from the Swiss Federal Statistical Office, which centrally processes all causes of death statements in Switzerland. For each fatality, doctors submit the immediate cause of death and zero, one or two co-morbidities to the authorities. Some doctors also submit more than two co-morbidities on the cause of death statement. Specialists at the Federal Office then use ICD-10 codes and ICD-10 combination rules to generate the cause of death database, that finally contains an immediate cause of death (listed as I) and zero, one or two co-morbidities (listed as II). For the current study, the processed data from the Swiss Federal Office was used, not the original cause of death statements.
Data were extracted from the Swiss statistics on causes of death for the years 1995 to 2007 and for residents of the Canton of Zurich (Switzerland). A total of 3431 cases of suicide (ICD-10 codes X60–X84) were listed in that period. Methods of suicide were grouped as follows: poisoning (X60–69.9); hanging, strangulation, suffocation, drowning (X70–71.9); firearm (X72–74.9); jumping from a high place (X80–80.9); jumping or lying before a moving object (X81–81.9); others (X75–79.9, X82–84.9).
On the basis of these data, suicide methods and co-morbidities were analysed. Descriptive statistics were used and results were presented as percentages. When two co-morbidities of the same category, such as mental and behavioural disorders, were noted for one person, they were counted only once to calculate their prevalence.
To calculate mean suicide rates for sex and age groups, permanent resident population counts of the years 1994 to 2007 were used (population at midyear, calculated as the average of the population at the end of two subsequent years). Children under 10 years of age were excluded as no suicide was documented in that age group.
Statistical modelling (see below) was applied to compare sociodemographic factors (sex, age group, marital status, religion, type of municipality) of suicide victims to the general population, for which data from the Swiss Federal Population Census of the year 2000 was used, which included 1.125 million residents in the Canton of Zurich (excluding children under the age of 10, visitors and holders of short stay permits).
All 171 municipalities of the Canton of Zurich were classified into seven categories according to the terminology of Schuler and Joye [23]. Industrial and tertiary municipality types were combined with suburban municipalities, agro-mixed with rural commuter municipalities, and Wetzikon was considered a suburban municipality. The following 5 groups resulted:
2 cities (Zurich and Winterthur), characterised by their large population (>50'000); 16 high-income municipalities, characterised by a high real income of inhabitants, and situated mostly at the borders of the lake of Zurich (including the so-called ‘gold coast’); 63 industrial, tertiary and suburban municipalities, characterised by a high percentage of secondary and tertiary sector economies and not exceeding a certain fraction of apartment buildings, respectively; 54 periurban municipalities, that lie within an agglomeration but do not fulfil the criteria for suburban or high-income municipalities; 36 agro-mixed and rural commuter municipalities, characterised by a relatively high percentage of primary sector economy and people living but not working there (commuters).
A logit model, which belongs to the family of generalised linear models and is used for binomial regression, was employed. Sex, age group, marital status, religion and place of residence (type of municipality) were chosen as categorical predictor variables, with suicide (1 or 0) as the response variable. Age was not used as a continuous variable, since it was not linear in the model. Therefore, 10 year age groups were chosen for all analyses. Calculating a model gives the possibility of looking at one predictor variable while adjusting for the others, for example looking at the effect of the marital status independently from the age group. Odds ratios (OR) and 95% confidence intervals (CI) were calculated from single factors of the logit function (for interpretation of ORs, see [24]). An alpha level of 0.05 was considered statistically significant.
SPSS Statistics version 17.0 (SPSS Switzerland, Zurich, Switzerland) was used for data evaluation. R version 2.8.1 (http://www.r-project.org) was used for modelling (function: glm).
Table 1 shows a statistically significant difference in suicide risk among sexes. The OR for women was 0.38 (95% CI 0.35–0.41), meaning women were 62% less likely to commit suicide than men. With increasing age, suicide risk increased. This was particularly evident in the age groups of 80–89 (OR 4.05, 95% CI 3.52–4.65) and 90 years and older (OR 4.93, 95% CI 4.00–6.07) compared to the reference group aged 40–49 (OR 1.00).
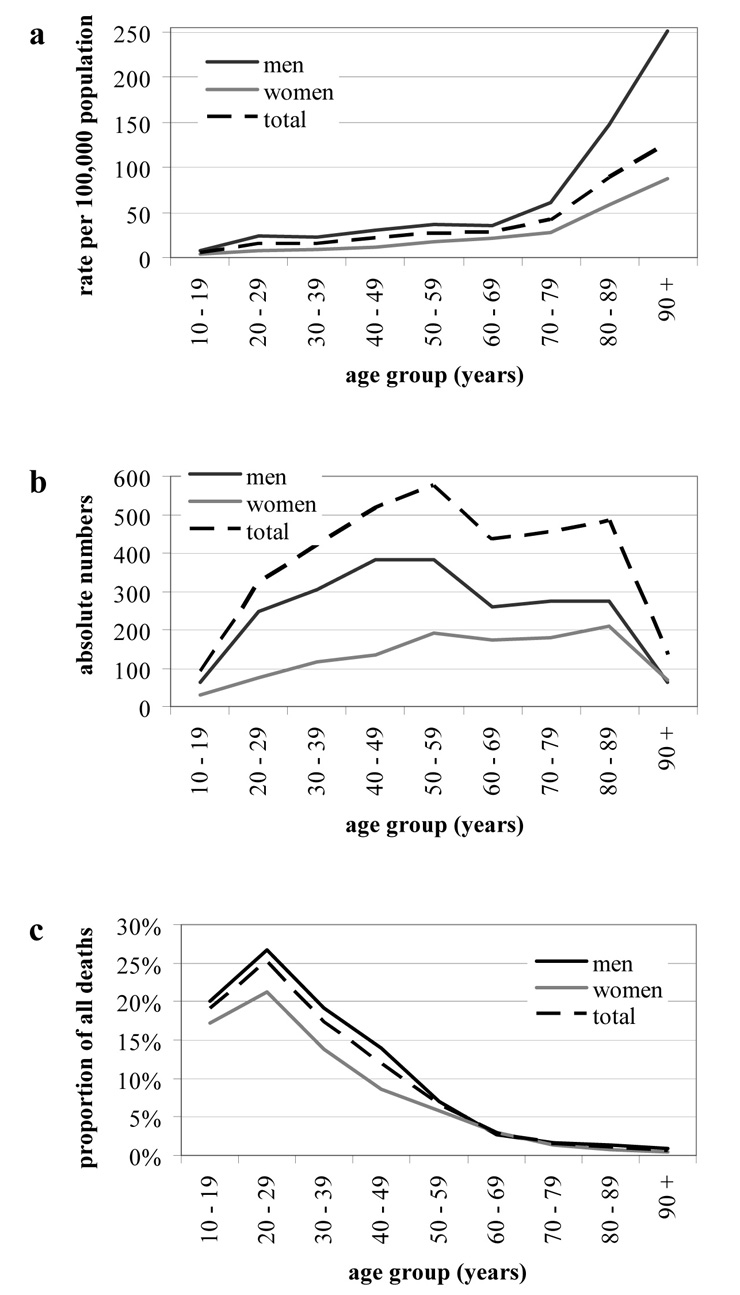
Figure 1
Mean suicide rates per year (a), suicide counts (b) and suicide proportions of all deaths (c) by age group and sex, in the Canton of Zurich, 1995–2007.
Married individuals had a significantly lower OR than single people. They were 55% less likely to kill themselves. Being divorced conferred a trend to a higher suicide risk than being single, but this was not statistically significant. Widowed persons still had a significantly reduced suicide risk relative to singles even though it was higher than the risk for married people. This effect only became apparent through statistical modelling. Crude suicide rates were highest for widowed and divorced people, with both groups being on average older than singles. Additionally considering interactions between sociodemographic factors in the model, widowed women showed a lower suicide rate compared to single women, whereas widowed men were more likely to kill themselves than single men.
Roman Catholics had a lower suicide risk than Protestants. No calculations for members of other religious groups in the Canton of Zurich (e.g. Jews or Muslims) could be made, since either only few people belonged to those groups or the religious affiliation was not known.
Living in the two largest cities (cantonal capital Zurich, Winterthur) or living in high-income municipalities conferred slightly higher suicide risks than living in industrial, tertiary or suburban municipalities. Inhabitants of the cities were also more likely to commit suicide than those of periurban municipalities. Agro-mixed and rural commuter municipalities were small and showed large variations, therefore no conclusions about their inhabitant's suicide risks could be drawn.
Figure 1a shows mean suicide rates per 100'000 people. The lowest rate was found in the age group of 10–19 years. While the suicide rate rose with age, its incline was steepest in high age up to rates of 148 (men, 80–89), 251 (men, 90+), 58 (women, 80–89) and 87 (women, 90+) per 100'000 people. Men in all age groups had a suicide rate two to three times that of women. In order to be able to compare our data to other studies, we calculated suicide rates per 100'000 people (including children of all ages). We found mean suicide rates per year in the Canton of Zurich to be 29.0 and 14.5 per 100'000 people for men and women, respectively.
Even though suicide rates rose with increasing age, the highest absolute numbers were found in the age group of 40–59 years for men and 50–89 years for women (fig. 1b). The average age of suicide victims was 55 for men and 61 for women. In absolute numbers, men were represented more frequently in all age groups except in the one of 90 years and older.
The percentage of suicide in all deaths was higher in younger people (fig. 1c). Over 25% of deaths in the age group of 20–29 years were the consequence of suicide; suicides made up 17% of deaths in the group of 30–39 years, and only 1.5% of people 70 years or older died due to suicide as other causes, mostly natural deaths, were far more common.
In total, the most popular method was poisoning followed by hanging, strangulation, suffocation or drowning and firearm suicide. Jumping from a high place or jumping or lying before a moving object and various other means, such as injury with a sharp object, fire or intentional crashing of motor vehicles, were less frequent. Delineation between accidents and suicides is not always obvious. Deaths after road traffic accidents, drowning or poisoning suicides may, in particular, have been underestimated.

Figure 2
Suicide rates per 100'000 people (age-specific, not considering children under 10 years of age) per method by sex, in the Canton of Zurich, 1995–2007.
Usage rates of chosen suicide methods varied with age (table 2) and sex (fig. 2, table 2). Poisoning was twice as common in women, shooting ten times as frequent in men. Jumping or lying before a moving object (mostly train suicides) accounted for 30% of male and 41% of female suicides under the age of 20. Men aged between 20 and 90 shot themselves more frequently than those younger or older. Poisoning became increasingly popular with increasing age.
Causes of death statistics do not only report cause of death but also list up to two co-morbidities (ICD-10). Mental illness constitutes a relevant diagnosis in suicide victims. Within the age group of 20–59 years, the proportion of mental illnesses such as depression, schizophrenia or alcoholism ranged between 41% and 45% and decreased with increasing age (table 3). In the age group of 10–19 years, mental and behavioural disorders accompanied almost a third of suicide cases, whereas two thirds remained without a listed co-morbidity.
Malignant tumours were found in 11% of the 50–59 year old and 30% of the 70–79 year olds. Nervous system disorders such as multiple sclerosis or Parkinson's disease amounted to 10% of the suicide victims aged 70–79. Diseases of the circulatory system were found increasingly in people aged 70 and older. No co-morbidities were listed for 43% of male and 28% of female suicide victims.
Overall male suicide rates showed a tendency to decline between 1995 and 2003, whereas male rates from 2004 to 2007 and female rates remained approximately constant. All four seasons showed a similar frequency in suicide. There were variations in suicide counts between single months: most suicides were committed in March, and least suicides were committed in October.
| Table 1Influence of sex, age, marital status, religion and place of residence on the suicide risk, in the Canton of Zurich (suicide victims 1995–2007 compared to population 2000). | ||||
| 95% confidence interval | ||||
| Odds ratio | Lower | Upper | p-value | |
| Sex | ||||
| Male | 1.00 | |||
| Female | 0.38 | 0.35 | 0.41 | < 0.0001 |
| Age group | ||||
| 10–19 | 0.16 | 0.13 | 0.20 | < 0.0001 |
| 20–29 | 0.47 | 0.40 | 0.54 | < 0.0001 |
| 30–39 | 0.61 | 0.53 | 0.69 | < 0.0001 |
| 40–49 | 1.00 | |||
| 50–59 | 1.27 | 1.13 | 1.43 | < 0.0001 |
| 60–69 | 1.46 | 1.28 | 1.66 | < 0.0001 |
| 70–79 | 2.02 | 1.77 | 2.30 | < 0.0001 |
| 80–89 | 4.05 | 3.52 | 4.65 | < 0.0001 |
| 90+ | 4.93 | 4.00 | 6.07 | < 0.0001 |
| Marital status | ||||
| Single | 1.00 | |||
| Married | 0.45 | 0.41 | 0.49 | < 0.0001 |
| Widowed | 0.87 | 0.76 | 0.99 | 0.038 |
| Divorced | 1.11 | 0.99 | 1.25 | 0.080 |
| Religion | ||||
| Protestant | 1.00 | |||
| Roman Catholic | 0.70 | 0.64 | 0.77 | < 0.0001 |
| Other, none | 0.97 | 0.90 | 1.06 | 0.50 |
| Type of municipality | ||||
| Industrial, tertiary and suburban municipalities | 1.00 | |||
| Periurban municipalities | 1.02 | 0.90 | 1.16 | 0.73 |
| Agro-mixed and rural commuter municipalities | 1.11 | 0.89 | 1.37 | 0.36 |
| High-income municipalities | 1.20 | 1.06 | 1.36 | 0.005 |
| Cities (Zurich, Winterthur) | 1.21 | 1.12 | 1.31 | < 0.0001 |
| Table 2 Suicide methods by sex and age group in percentages, in the Canton of Zurich, 1995–2007. | ||||||||||
| Men | 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | 90+ | All |
| Poisoning | 1.6% | 9.3% | 16.1% | 19.2% | 17.0% | 27.6% | 40.4% | 39.8% | 48.4% | 23.7% |
| Hanging, strangulation, suffocation, drowning | 38.1% | 25.1% | 26.2% | 32.5% | 29.2% | 21.8% | 18.2% | 15.3% | 18.8% | 25.0% |
| Firearm | 15.9% | 49.0% | 34.4% | 30.2% | 36.0% | 26.8% | 28.0% | 27.4% | 7.8% | 31.8% |
| Jumping from a high place | 12.7% | 7.7% | 6.9% | 6.6% | 4.7% | 10.0% | 6.9% | 9.1% | 23.4% | 7.8% |
| Jumping or lying before moving object | 30.2% | 5.3% | 8.9% | 6.3% | 8.1% | 9.2% | 2.9% | 3.6% | 1.6% | 7.0% |
| Others | 1.6% | 3.6% | 7.5% | 5.2% | 5.0% | 4.6% | 3.6% | 4.7% | 0.0% | 4.7% |
| Women | 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | 90+ | All |
| Poisoning | 20.7% | 33.3% | 31.6% | 37.3% | 39.6% | 54.0% | 65.7% | 72.7% | 77.1% | 51.9% |
| Hanging, strangulation, suffocation, drowning | 6.9% | 30.7% | 29.1% | 26.1% | 26.0% | 21.8% | 18.5% | 15.3% | 8.6% | 21.5% |
| Firearm | 10.3% | 6.7% | 7.7% | 2.2% | 4.2% | 2.9% | 0.6% | 0.5% | 0.0% | 3.0% |
| Jumping from a high place | 20.7% | 13.3% | 14.5% | 14.9% | 13.0% | 12.6% | 9.0% | 8.6% | 8.6% | 11.9% |
| Jumping or lying before moving object | 41.4% | 16.0% | 12.0% | 12.7% | 13.5% | 6.9% | 2.8% | 1.4% | 0.0% | 8.6% |
| Others | 0.0% | 0.0% | 5.1% | 6.7% | 3.6% | 1.7% | 3.4% | 1.4% | 5.7% | 3.2% |
| Table 3 Co-morbidities in suicide victims by age group in percentages, in the Canton of Zurich, 1995–2007. | ||||||||||
| 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | 90+ | All | |
| Malignant neoplasms | 1.1% | 0.6% | 1.2% | 3.3% | 10.6% | 22.1% | 30.0% | 18.0% | 14.9% | 12.4% |
| Mental and behavioural disorders | 29.3% | 41.0% | 44.8% | 45.4% | 42.4% | 34.5% | 25.2% | 26.9% | 18.7% | 36.3% |
| Diseases of the nervous system | 0.0% | 0.3% | 1.7% | 3.1% | 4.2% | 6.7% | 10.2% | 6.2% | 3.0% | 4.6% |
| Diseases of the circulatory system | 0.0% | 0.0% | 0.5% | 1.4% | 2.8% | 3.0% | 13.2% | 17.2% | 22.4% | 6.1% |
| None specified | 68.5% | 54.3% | 48.3% | 41.7% | 37.9% | 32.0% | 23.2% | 29.4% | 30.6% | 37.9% |
We found mean suicide rates in the Canton of Zurich of 29.0 and 14.5 per 100'000 people for men and women, respectively. This amounted to a rather low male/female suicide ratio of 2.0 compared to the other Swiss cantons, where ratios range from 1.4 (Canton of Zug) to 4.3 (Canton of Appenzell Inner Rhodes) [1]. Regarding the WHO statistics [25], our findings and Swiss suicide rates (men: 26.5, women: 10.0) are comparable to those of neighbouring countries including Germany (men: 20.2, women: 7.3), Austria (men: 27.3, women: 9.8) and France (men: 26.1, women: 9.4), while Italy shows lower rates (men: 11.1, women: 3.4).
In the current data, the highest two age groups (80–89 and 90+ years) present suicide rates (148 and 251 per 100'000 people for men, and 58 and 87 for women) that are high even in an international comparison. Suicide rates have been reported previously to rise with increasing age. For example, in England and Wales the age group of 80–89 years was reported to have a suicide rate of 14–18 (men) and 3–4 (women) per 100'000 people, whereas the group of 90 years and older had a suicide rate of 24 (men) and 4 (women) [4]. A similarly sharp rise with increasing age was reported in China (up to 165 for men and 122 for women over 85 in rural areas) [5] and in the USA (75 for men and 6 for women over 85) [2].
Our model shows, for residents of the Canton of Zurich, that married and, to a minor degree, widowed people are less likely to kill themselves than single people, whereas divorced people have a higher tendency for suicide than single people, although this was not statistically significant. These findings showing this protective aspect of marriage are in line with other studies [6, 9].
According to our results, Roman Catholics are about 30% less likely to commit suicide than Protestants in the Canton of Zurich, a finding which is not new. Data from one of the right-to-die organisations in Switzerland showed that more people from Protestant than Catholic cantons utilised assisted suicide [26]. In an American study, county groups with higher percentages of Catholics reported the lowest suicide rates, whereas various Protestant denominations ranked higher [27]. Relevant factors in this context may be denial and underreporting of suicides [28], better coping mechanisms or better community support. Lower suicide rates are also being argued to result from an association of religious belief with lower tolerance of suicide [29]. Religious affiliation in depressed inpatients is generally associated with reporting of less suicidal behaviour [30].
Underreporting of suicides among Catholics may be a problem; its magnitude is estimated to range between 20 and 30% [28]. We do not feel this is an issue that is that extensive, nor that it is particularly restricted to Catholics. Our system does not allow suicides that cause visible problems, such as blocking a train for hours, to be underreported. In today's modern world of life insurance, underreporting of suicides should also not be expected to be a phenomenon restricted to any specific religious group. Also, wrongly submitting an accident or natural death as a suicide on the cause of death statement cannot be seen as a gross error if the situation does not provide any particular clues that indicate a suicide. Reliability of cause of death data can be greatly improved by summoning experts to detail circumstances, by determining patient history and recent history by interviewing family, neighbours and workmates, by conducting autopsy and ancillary tests and by then issuing a report after thorough analysis.
It is not obvious why people in urban or rich communities kill themselves more often. In the Canton of Zurich, cities and high-income municipalities lead the statistics of suicide rates. Industrial, tertiary and suburban municipalities have the lowest rate, and the numbers of small rural municipalities have a large variation and are therefore not significantly different from the other types. It has been shown previously that among people with a history of mental illness, those with a higher income are at greater risk of committing suicide compared to those with a lower income [31]. In contrast, richer people in the general population have a lower suicide rate. So it appears that richer people with a mental illness may be more suicidal because they may feel more stigmatised, vulnerable and shameful about having a mental illness [32]. This interpretation of increased suicide rates found in high-income municipalities has to be weighed cautiously since personal income of individual suicide victims in our data is unknown. Nevertheless, it has to be accepted that stigmatisation of mental illness is a relevant factor in our society [33, 34]. In addition, our higher urban suicide rates are not in line with findings from other countries, where suicide risk is larger in rural areas [5, 35, 36].
Data presented here pertains to the Canton of Zurich. However, we suggest that the analysis may well find relevance across the borders of our canton. The Canton of Zurich (ZH) compares to Switzerland (CH) with regard to a number of relevant rates; age distribution (0–19 years: CH: 22.9%, ZH: 20.5%; 20–64 years: CH: 61.8%, ZH: 64.4%; >64 years: CH: 15.4%, ZH: 15.0%), persons per household (CH: 2.2%, ZH: 2.1%), unemployment rate (CH: 2.8%, ZH: 2.6%), proportion of foreigners (CH: 21.1%, ZH: 22.9%) and living density (residents per room) (CH: 0.59, ZH: 0.58) [37]. However, there are also differences to the other cantons, for example the Canton of Zurich has the largest population and two large cities, in which we found higher suicide rates than in the industrial, tertiary or suburban municipalities.
It appears that methods can be ranked as first choice methods (such as firearms or poisoning, which are believed to be particularly effective) as opposed to so-called replacement methods (hanging or widely available methods such as jumping or lying in front of a moving object that carry a risk of prolonged agony or even survival). In our data, the most common method was poisoning followed by hanging, strangulation, suffocation or drowning and firearm suicide.
We found usage of poison to be increasingly frequent with age. Poisoning leads the statistics in men over 60 and women over 20, and is used about twice as frequently in women as in men. It has to be noted that our data also include assisted suicides, where poisoning is the predominant method and the majority of cases are women [38]. Assisted suicides are legal in Switzerland and supported by several right-to-die organisations [26], but could not be analysed separately, since these cases were not identifiable in our data.
Firearms suicide is the most common method among younger men according to the current data (most popular method for men aged 20–39 years). In the region of Basel, it is the most frequent suicide method overall [22].
Hanging is the most prevalent suicide method in Europe, accounting for almost 50% of suicides [39], and can be regarded as a replacement method when other means are not available. Highest percentages of strangulation among all suicides are reported from eastern European countries with rates up to 91.7% in Lithuania [21]. In our data, hanging, strangulation, suffocation and drowning were not found quite as often; they were used in 6.9 to 38.1% of the cases, depending on sex and age group.
Generally, an effective restriction to access a particular means for suicide is thought to be able to save lives, for example regional availability of high bridges correlates positively with high rates of suicide by jumping. While statistically men appear to substitute jumping with poisoning in regions of relatively scarce bridges, women's suicide rates reflect no method substitution [10]. As our region does not seem to feature as many high publically available architectural structures as others, suicides due to jumping (7.8%) were not as frequent as for example in Malta, Luxembourg or Spain [21].
In the age groups of 50–59 years and 60–69 years, we found 10.6% and 22.1% of suicide victims to suffer from malignant neoplasms. The age between 50 and 70 may be a critical age for newly diagnosed cancer; in a multiethnic study, total cancer peak incidence appears to range between age 56 and 62 [40]. In Switzerland, incidence of cancers generally rises from age 45 onwards, with considerable differences in age-incidence correlation among various types of cancer [41]. Additionally two studies, one in the Canton of Vaud and one in central Italy, showed elevated suicide risks for patients diagnosed with cancer, especially within the first year after diagnosis [13, 14].
In total, 36% of suicide victims were recorded to have a mental disorder, which was a rather low percentage compared to other studies that estimate 40 to 90% [4, 6, 42]. Some authors even assume suicide to be impossible without mental illness; one case-controlled study reported 97 to 100% of suicide victims to have a diagnosed mental illness [43]. The Zurich cohort study, that investigated the prevalence of mental disorders in a cohort of young adults, reported a 20 year cumulative prevalence rate for mood disorders of 24.2% and for total mental disorders of 48.6% in the general population [44]. In our data, 41.0% and 44.8% of the 20–29 and 30–39 year old suicide victims were listed as having had a mental disorder. However, regarding the literature, which shows higher suicide rates for patients with mood disorders [45, 46], higher percentages of mental disorders would have been expected in our sample.
Apart from being rather low, percentage of reported mental illness in suicide victims in our data declines with age. This is interesting as depression is regarded as the most significant risk factor for suicide in old age [11, 42]. However, mental illness in the elderly can lead to a complex clinical picture that may remain poorly recognised and treated: co-occurring illnesses with overlapping symptoms such as loss of appetite, lack of energy or insomnia and a tendency of physicians to regard late-life depression as a normal response to multiple life changes such as being on a low fixed income, loss of purpose, isolation, death of a spouse, onset of multiple illnesses or increasing dependency needs [47]. Recognition and appropriate reporting and coding of depression – particularly late in life – may also carry significant economical relevance: when compared to non-depressed individuals, after controlling for age and co-morbid medical illnesses, those with depression had almost twice as many primary care visits, twice as many referrals to specialists, and not only more than twice as many radiological tests but also higher total charges and almost twice as high outpatient charges [48].
In accordance to data from throughout Switzerland [1], in the Canton of Zurich male suicide rates showed a tendency to decline between 1995 and 2003 and then to stay constant to 2007. Over the same period, female rates remained approximately constant, resulting in a trend towards a slightly declining overall suicide rate despite an increase in assisted suicides and more people depending on social welfare [49]. Unemployment and low socioeconomic status are known additional suicide risk factors [16, 50], although socioeconomic status as a risk factor can lose relevance when corrected for mental illness and suicide in the family [51]. Trends for the future are unclear. With more people in higher age groups due to demographic changes in the coming years [52], suicide rates may rise again.
Self damaging behaviour is a relevant issue in Switzerland. As another example, hospital diagnoses related to alcohol between age 14 and 19 are considerably higher in Switzerland compared to both Germany and Austria, and are interpreted as being related to other mental illnesses or conditions [53]. As there are preventive measures in place to reduce alcohol abuse, such as binge drinking, in young people, it may be appropriate to consider specific measures regarding suicides.
In addition to previously established preventive aspects – reducing access to firearms, illicit or prescription drugs – and based on our analysis, we consider the following as potentially promising fields of additional preventive activity:
The current data, with a trend to higher suicide rates in cities on one hand and rich municipalities on the other hand, can be interpreted in context of related current literature in that reduction of stigmatising aspects of mental illness on a societal level could be a relevant step towards suicide prevention. In particular, our society tends to value ‘high performance’ to a higher degree than to consider what an average individual may be able to cope with mentally [54]. Unique types of intense stress are known to be associated with increased suicide rates such as the Japanese ‘examination hell’ and its association with suicide of young people [55], or the combination of low social support, long working hours and heavy workloads [56], obviously without any other outlet for the accumulated aggression besides suicide. To work towards a wider acceptance of mental issues in context of a high performance society may save lives.
We believe that in our data, relatively low reported rates of mental illness in the elderly and very high suicide rates of the elderly represent a contrast. Medical skill training to recognise or disambiguate co-morbidity overlap in depressed elderly people could be helpful to reduce depression, suicide rates and costs, since depression has been found to be associated with significantly greater utilisation of ambulatory care, and with higher costs for blood tests, radiologic tests and consultations, even after adjustment for age, gender, co-morbidity, insurance status and primary care provider [48].
There are several limitations of this analysis that could be addressed in future studies. Regarding sociodemographic variables, it might be valuable to look at changes in the marital status (i.e. the time span between a divorce or death of a spouse) and a suicide. The impact of co-morbidities could be investigated more deeply, if more data were available: in the data set, the number of co-morbidities is presently limited to two, which might not be sufficient. Also, prevalence rates for disorders, especially mental and behavioural disorders, for all age groups in the general population are lacking for comparison. In addition, the implications of assisted suicide on the suicide rates and methods of the ill and elderly remain unclear and require further investigations.
We are grateful to Peter Moser for valuable and helpful input.
1 Swiss Health Observatory. 2.3.2 Suizide und Suizidversuche. 2009 May [cited 2009 Sep 02]. Available from: http://www.obsandaten.ch/indikatoren/2_3_2/2006/d/232.pdf
2 Murphy GE. Why women are less likely than men to commit suicide. Compr Psychiatry. 1998;39(4):165–75.
3 Rich, CL, Ricketts, JE, Fowler, RC, Young, D. Some differences between men and women who commit suicide. Am J Psychiatry. 1988;145(6): 718–22.
4 Shiner M, Scourfield J, Fincham B, Langer S. When things fall apart: Gender and suicide across the life-course. Soc Sci Med. 2009;69(5):738–46.
5 Phillips MR, Li X, Zhang Y. Suicide rates in China 1995–99. Lancet. 2002;359(9309):835–40.
6 Wanta BT, Schlotthauer AE, Guse CE, Hargarten SW. The burden of suicide in Wisconsin's older adult population. WMJ. 2009;108(2):87–93.
7 Shah A. The relationship between suicide rates and age: an analysis of multinational data from the World Health Organization. Int Psychogeriatr. 2007;19(6):1141–52.
8. Durkheim É. Le suicide. Étude de sociologie. 1897 [cited 2009 Sep 04]. Available from: http://classiques.uqac.ca/classiques/Durkheim_emile/suicide/suicide.html
9 Lorant V, Kunst AE, Huisman M, Bopp M, Mackenbach J, EU Working Group. A European comparative study of marital status and socio-economic inequalities in suicide. Soc Sci Med 2005;60(11):2431–41.
10 Reisch T, Schuster U, Michel K. Suicide by jumping and accessibility of bridges: results from a national survey in Switzerland. Suicide Life Threat Behav. 2007;37(6):681–7.
11 Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193–204.
12 Flensborg-Madsen T, Knop J, Mortensen EL, Becker U, Sher L, Grønbaek M. Alcohol use disorders increase the risk of completed suicide – irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Res. 2009;167(1–2):123–30.
13 Levi F, Bulliard JL, La Vecchia C. Suicide risk among incident cases of cancer in the Swiss Canton of Vaud. Oncology. 1991;48(1):44–7.
14 Crocetti E, Arniani S, Acciai S, Barchielli A, Buiatti E. High suicide mortality soon after diagnosis among cancer patients in central Italy. Br J Cancer. 1998;77(7):1194–6.
15 Denney JT, Rogers RG, Krueger PM, Wadsworth T. Adult suicide mortality in the United States: marital status, family size, socioeconomic status, and differences by sex. Soc Sci Q. 2009;90(5):1167.
16 Inoue K, Tanii H, Abe S, Nishimura Y, Kaiya H, Nata M, et al. The report in the correlation between the factor of unemployment and suicide in Japan. Am J Forensic Med Pathol. 2008;29(2):202–3.
17 Kanchan T, Menon A, Menezes RG. Methods of choice in completed suicides: gender differences and review of literature. J Forensic Sci. 2009;54(4):938–42.
18 Wiebe DJ. Guns in the home: risky business. LDI Issue Brief. 2003;8(8):1–4.
19 Killias M. International correlations between gun ownership and rates of homicide and suicide. CMAJ. 1993;148(10):1721–5.
20 Ajdacic-Gross V, Killias M, Hepp U, Gadola E, Bopp M, Lauber C, et al. Changing times: a longitudinal analysis of international firearm suicide data. Am J Public Health. 2006;96(10):1752–5.
21 Ajdacic-Gross V, Weiss MG, Ring M, Hepp U, Bopp M, Gutzwiller F, et al. Methods of suicide: international suicide patterns derived from the WHO mortality database. Bull World Health Organ. 2008;86(9):726–32.
22 Frei A, Han A, Weiss MG, Dittmann V, Ajdacic-Gross V. Use of army weapons and private firearms for suicide and homicide in the region of Basel, Switzerland. Crisis. 2006;27(3):140–6.
23 Schuler M, Joye D. Typologie der Gemeinden der Schweiz: 1980 – 2000. Swiss Federal Statistical Office [cited 02 Sep 2009]. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/regionen/11/geo/raeumliche_typologien/01.parsys.0003.downloadList.00031.DownloadFile.tmp/typocommtextde.pdf
24 Hailpern SM, Visintainer PF. Odds ratios and logistic regression: further examples of their use and interpretation. The Stata Journal. 2003;3(3):213–25.
25 WHO. Suicide rates. 2003 May [cited 2009 Sep 02]. Available from: http://www.who.int/mental_health/prevention/suicide/suiciderates/en/
26 Bosshard G, Ulrich E, Bär W. 748 cases of suicide assisted by a Swiss right-to-die organisation. Swiss Med Wkly. 2003;133(21–22):310–7.
27 Pescosolido BA, Georgianna S. Durkheim, suicide, and religion: toward a network theory of suicide. Am Sociol Rev. 1989;54(1):33–48.
28 Connolly JF. Suicide and the Irish problem: Comments on under-reporting. Arch Suicide Res. 1997;3:25–9.
29 Neeleman J, Halpern D, Leon D, Lewis G. Tolerance of suicide, religion and suicide rates: an ecological and individual study in 19 Western countries. Psychol Med. 1997;27(5):1165–71.
30 Dervic K, Oquendo MA, Grunebaum MF, Ellis SE, Burke AK, Mann JJ. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161(12):2303–8.
31 Agerbo E, Mortensen PB, Eriksson T, Qin P, Westergaard-Nielsen N. Risk of suicide in relation to income level in people admitted to hospital with mental illness: nested case-control study. BMJ. 2001;322(7282):334–5.
32 Penn DL, Martin J. The stigma of severe mental illness: some potential solutions for a recalcitrant problem. Psychiatr Q. 1998 Fall;69(3):235–47.
33 Kurt H. Über Scheininvalide und Psychiater… Schweizerische Ärztezeitung. 2007;88(23):1000–2.
34 Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–20.
35 Kapusta ND, Zorman A, Etzersdorfer E, Ponocny-Seliger E, Jandl-Jager E, Sonneck G. Rural-urban differenced in Austrian suicides. Soc Psychiatry Psychiatr Epidemiol. 2008;43(4):311–8.
36 Yip PS, Callanan C, Yuen HP. Urban/rural and gender differentials in suicide rates: east and west. J Affect Disord. 2000;57(1):99–106.
37 Swiss Federal Statistical Office, Regional Comparator [cited 2010 Apr 05]. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/regionen/regionalportraets/comparator.html
38 Fischer S, Huber CA, Imhof L, Mahrer Imhof R, Furter M, Ziegler SJ, Bosshard G. Suicide assisted by two Swiss right-to-die organisations. J Med Ethics. 2008;34:810–4.
39 Värnik A, Kõlves K, van der Feltz-Cornelis CM, Marusic A, Oskarsson H, Palmer A, et al. Suicide methods in Europe: a gender-specific analysis of countries participating in the "European Alliance Against Depression". J Epidemiol Community Health. 2008;62(6):545–51.
40 Kolonel LN, Altshuler D, Henderson BE. The multiethnic cohort study: exploring genes, lifestyle and cancer risk. Nat Rev Cancer. 2004;4(7):519–27.
41 Swiss Association of Cancer Registries. Switzerland – statistics of cancer incidence 1986–2005. 2007 Dec [cited 2009 Sep 02]. Available from: http://www.asrt.ch/asrt/newstat/in4ch8605.pdf
42 Stoppe G. Depression in old age. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2008;51(4):406–10.
43 Cheng AT. Mental illness and suicide. A case-control study in east Taiwan. Arch Gen Psychiatry. 1995;52(7):594–603.
44 Angst J, Gamma A, Neuenschwander M, Ajdacic-Gross V, Eich D, Rössler W, Merikangas KR. Prevalence of mental disorders in the Zurich Cohort Study: a twenty year prospective study. Epidemiol Psichiatr Soc. 2005;14(2):68–76.
45 Angst J, Angst F, Stassen HH. Suicide risk in patients with major depressive disorder. J Clin Psychiatry. 1999;60(Suppl 2):57–62.
46 Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord. 2002;68(2–3):167–81.
47 Borja B, Borja CS, Gade S. Psychiatric emergencies in the geriatric population. Clin Geriatr Med. 2007;23(2):391–400, vii.
48 Luber MP, Hollenberg JP, Williams-Russo P, DiDomenico TN, Meyers BS, Alexopoulos GS, et al. Diagnosis, treatment, comorbidity, and resource utilization of depressed patients in a general medical practice. Int J Psychiatry Med. 2000;30(1):1–13.
49 Bentz D, Gerber V, Priester T, Gruber B, Ruch T, Jankowski T, et al. Sozialbericht Kanton Zürich 2007. 2008 [cited 2009 Sep 02]. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/13/22/publ.Document.113856.pdf
50 Beautrais AL, Joyce PR, Mulder RT. Youth suicide attempts: a social and demographic profile. Aust N Z J Psychiatry. 1998;32(3):349–57.
51 Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. BMJ. 2002;325(7355):74–8.
52 Bucher H-P. Babyboomer kommen ins Rentenalter. statistik.info 06/08. 2008 Jun [cited 2009 Sep 21]. Available from: http://www.statistik.zh.ch/themenportal/themen/down.php?id=2152&fn=2008_06.pdf
53 Gmel G, Kuntsche E. Alkohol-Intoxikationen bei Jugendlichen und jungen Erwachsenen. Eine Analyse der Schweizer Krankenhausstatistik. Abhängigkeiten. 2007;1/07:36–49.
54 Brühlmann T. Psychiatrische Hospitalisation als Rettungsanker in einer Hochleistungsgesellschaft – eine neue Indikation zur stationären Behandlung. Schweizerische Ärztezeitung. 2009;90:184–7.
55 Iga M. Suicide of Japanese youth. Suicide Life Threat Behav. 1981;11(1):17–30.
56 Amagasa T, Nakayama T, Takahashi Y. Karojisatsu in Japan: characteristics of 22 cases of work-related suicide. J Occup Health. 2005;47(2):157–64.
No funding; no competing interests.