Primary care emergency services utilisation in German speaking Switzerland
DOI: https://doi.org/10.4414/smw.2010.13111
U
Güntensperger, R
Pinzello-Hürlimann, A
Ciurea, B
Muff, JP
Gutzwiller
Summary
BACKGROUND: Traditionally, emergency consultations have been done by a general practitioner (GP) in Switzerland. Over the last years, there seems to have been a shift between general practice to hospital emergency ward utilisation. There are several local initiatives of general practitioners and hospitals to change the organisation of emergency care. To plan a new organisation form of emergency care, delivery should be based on population based data.
OBJECTIVE: The aim of the study was to investigate the epidemiology and distribution of emergency consultations of primary care in a hospital and in a practice of general practitioners. In addition, factors of clinical performance in emergency consultations are of great public health interest.
METHODS: For this survey, all emergency patient contacts of general practitioners from the catchment area of Bülach, serving 27 088 inhabitants, were assessed by a questionnaire during the fourth quarter of 2006. Sex, age, time, duration of the contact and triage diagnosis were assessed. In addition, all patients seen by the emergency ward at the local hospital were assessed. Contact rates and hospitalisation rates per 100 000 inhabitants were determined. In addition, a multiple linear regression model was performed to determine factors associated with consultation time as a marker for clinical performance.
RESULTS: Between October 1th and December 31th 2006, 1001 patient contacts were registered at the same time period in the hospital and general practice. The patient contact rate was 94.8 contacts per 100 000 inhabitants per day, and the hospitalisation rate was 9.1 patient per 100 000 inhabitants. Patients seen at the hospital were older than in general practice (41.2 ± 22.8 vs. 32.6 ± 26.3 years) and consultation and waiting time was longer in the hospital than consultation time with the GP (144.8 ± 106.5 vs. 19.6 ± 17.6 minutes).
CONCLUSION: Nearly 1 out of 1000 inhabitants were looking for emergency primary care help, and 10% of the patients were seen urgently by general practitioners and hospital staff and were hospitalised. These numbers are important information for planning emergency primary care facilities. The most prevalent triage diagnoses in practice are infections, traumatological reasons and ENT-problems, whereas in hospital the most frequent triage diagnosis is a traumatological disorder, followed by thoracic pain and infections. In addition, GP’s treat patients more rapidly than a hospital does and treat patients in shorter time intervals.
A population-based cross-sectional study
Introduction
Traditionally in Switzerland, in a medical emergency the local general practitioner (GP) on call is contacted first. This contact is generally done by a direct phone call from the patient and if the GP estimates that it is necessary, the patient is seen in the GP practice afterwards. In the minority of cases, if the GP estimates that the hospital should be in charge of this case, patients are sent to the hospital. Recently, there is a trend that patients directly contact the hospital or present themselves at the emergency ward of a hospital, leading to an overflow of patients in emergency wards of hospitals. This trend has also been reported outside of Switzerland [1, 2]. In Switzerland, first reports described an increasing use of emergency departments in the 1990’s [3]. This report suggested, as one of the possible reasons, that immigrants not familiar with the Swiss health system were responsible for this trend. This hypothesis was confirmed by a study performed by general practitioners, who determined that 80% of cases looking for advice at the emergency department of a hospital did not have a serious medical problem and could have been managed by a general practitioner [4]. To highlight the importance of this topic in medicine, there are reports in Switzerland measuring different parameters of performance of emergency care departments of Swiss hospitals [5]. Possible reasons for this phenomenon are less GP’s than in the past and changing habits of the Swiss population seeking medical advice. Several reports published by GP’s discuss an increase in their work burden due to the diminished number of practitioners, due to a specialisation of younger fellows and an increased demand by the population. At the moment, it is unclear how many emergency contacts per inhabitant take place in Switzerland. There are reports describing the organisation of emergency primary care in Switzerland, which exists in different forms due to the federal health system [6]. This information was based upon questionnaires distributed to regional governments, and local GP groups. This study revealed 12080 patient contacts per 100 000 inhabitants per year, which approximately results in 33.5 patient contacts per 100 000 inhabitants per day. Another study which focused on costs of primary care, showed 41.6 patient contacts per 100 000 inhabitants per day [7]. This study used the administration software of the GP’s, but did not take phone calls into consideration. In addition, this study did not take account of hospital data and therefore, the number of patient contacts looking for urgent ambulatory care cannot be estimated from this survey. Another study analysed the different health problems and distribution of patients over the day, but it is impossible to calculate a patient contact rate from this data, because the population served by this group and the working days were not known [8]. All these studies have in common that simultaneous hospital data and data obtained by the GP’s were not been obtained, making a calculation of total patient contacts per day and population impossible. However, this is a parameter which is an absolute condition to plan a health system which covers the health care demands of the population.
Therefore, we conducted a population-based study based on information from GP’s, including hospital data collected in the same time interval. The aim of the study was to assess the total burden of primary ambulatory emergency care consisting of out-of-hours service in general practice provided by general practitioners and the primary care service in the hospital. A further aim of the study was to investigate the hypothesis that GP’s have a better clinical performance in taking decisions in urgent primary care than hospital staff.
Patients and methods
The study was performed by the Büli-Aerzte, which is an association by the local practitioners from the communities Bülach, Winkel, Bachenbülach, Hochfelden and Höri and is responsible for the organisation of the emergency medical service of the region. The health system of this area allows all inhabitants of these five communities to consult the practitioner in charge for 24 hours a day during weekends and Thursdays. On Mondays to Wednesdays and on Fridays, the general practitioner attended emergencies by himself, and the night was covered by a small group of colleagues (4–6 GP’s) in a rotation system. The population living in these five communities was obtained by the official census data of the canton of Zürich in 2006 and was at that time 27088 inhabitants [9]. Between October 1th and December 31th 2006, all emergency contacts between the general practitioner and patients were assessed by the practitioner on duty in the emergency medical service of Bülach. Patients seeking medical advice called a central number, used for emergencies only, and were connected directly to the GP on duty. At the practitioner’s practice, only three days a week were registered during the study, as was the usual practitioner’s emergency service organised at that time (e.g., Thursdays Saturdays and Sundays). Almost all GP’s reduced their regular consultation hours to a negligible amount. Not only patients seen in the doctor’s practice but also patients consulted on the phone were assessed, and time of consultation (time between walk in and walk out in minutes), duration of patient contact (= eye contact between patient and GP in minutes), patient demographics such as sex (male/female) and age (years), estimation of emergency status by the GP on call (estimated emergency by GP yes/no), hospitalisation (yes/no) and finally an estimation of the diagnosis by the GP on call (free text) were assessed.
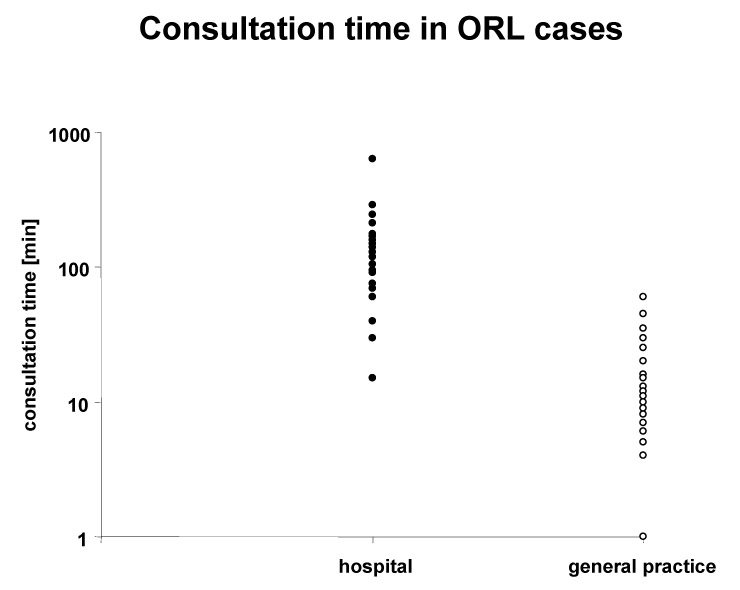
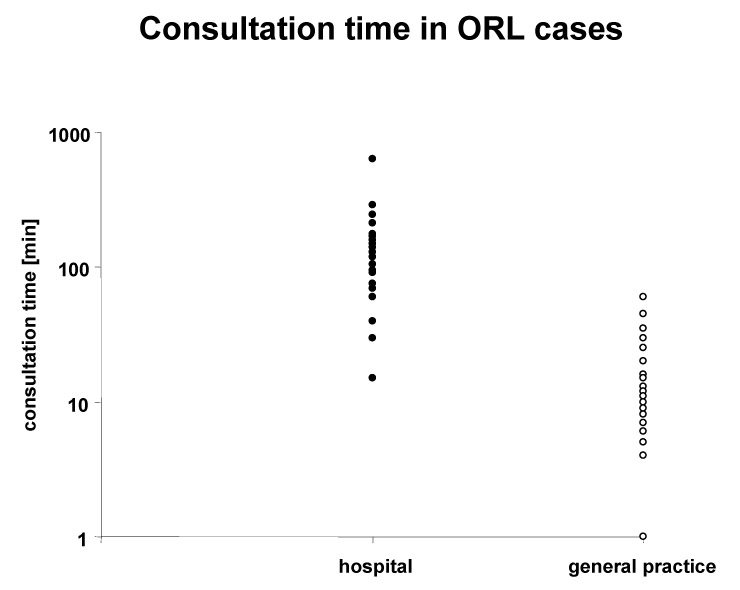
Figure 1
Consultation time as a marker for clinical performance at the emergency ward (hospital) and general practice. Only outpatients attending for ENT reasons were taken into analysis. There was a statistical significant and clinically relevant difference in consultation time (mean, SEM): 144.3 ± 22.7 min [hospital] vs. 16.6 ± 0.9 min [general practice], p <0.0001 (Wilcoxon signed rank).
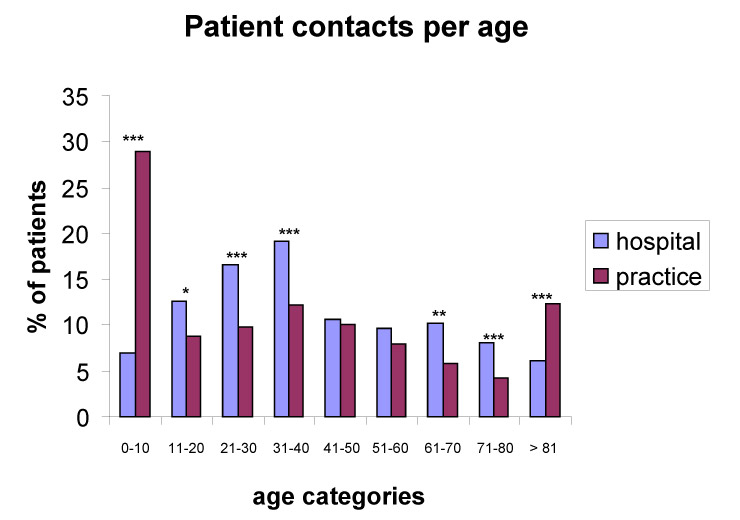
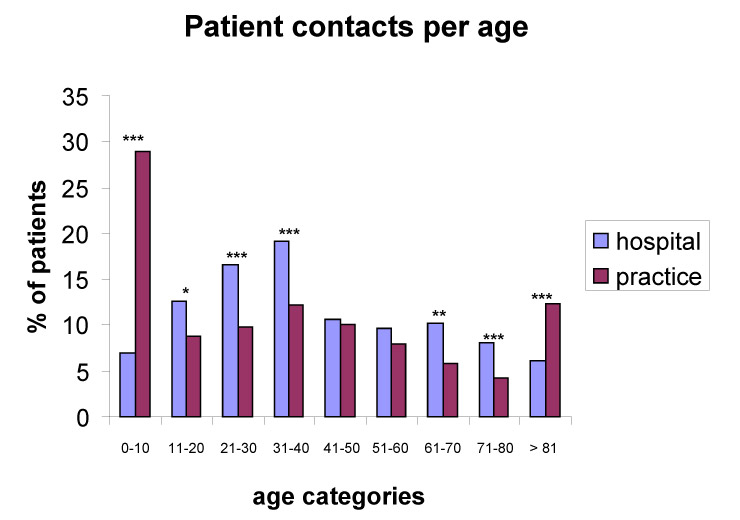
Figure 2
Distribution of patients according to age, seen at the emergency ward and by general practitioner, respectively. Differences marked are statistically significant: *p <0.05, **p <0.01, ***p <0.001.
In addition after completion of the data explained above, data of all counselling visits in the emergency ward of the local hospital were obtained. Only people who attended the hospital and lived in the five communities mentioned above were taken into account and analysed. Similarly as for the practitioners data, the hospital data contained age, sex, contact time and estimated diagnosis. For the epidemiological analysis, we only considered hospital data on Thursdays, Saturdays and Sundays to be comparable with the practitioner’s data. For the rest of the calculations, all data available (not only on Thursdays, Saturdays and Sundays) were used. Data sets were pooled and analysed together simultaneously.
The data were anonymous to the study investigators and upon contacting the ethical commission of the university hospital of Zürich, a written informed consent was not necessary to obtain.
Study design
This was a cross-sectional study analysing all emergency consultations to general practitioners and a hospital emergency ward between October 1th and December 31th 2006. As only patient data from patients living in the five communities mentioned above at one timepoint were analysed, the data can be viewed as population based cross-sectional data.
Outcome parameters
From the data obtained, patient contacts per 100 000 inhabitants, and patient needing hospitalisation per 100 000 inhabitants were calculated. Consultation time was considered to be a value of clinical performance. Triage diagnoses were assessed. ENT outpatients were defined to compare clinical performance of hospital and general practice looking at total in hospital time and consultation time, respectively. ENT outpatients were taken as examples for comparison, because the prevalence of ENT patients is very high in primary care: 32.6% of patients consult their GP in the UK [10]. As the duration of patient contact of the hospital physician on call was not available, total in hospital time (time between walk in and walk out in minutes) was taken in the hospital data set.
For multiple linear regression analysis, consultation time was defined as the dependent variable.
Independent variables
The different estimation diagnoses were taken as an independent variable, as well as age, sex, place of consultation (doctor’s practice vs. hospital), time of consultation, estimation of emergency status by the GP (yes/no) and hospitalisation (yes/no).
Statistical analysis
Microsoft Excel 2003 was used to calculate the descriptive statistics for contact per 100 000 inhabitants and hospitalisation per 100 000 inhabitants. To compare consultation time between patients attended at the hospital and patients attended at the practice of a GP, QQ-plots were performed to test for normal distribution of consultation time and in-hospital time, respectively. In case of normal distribution, student t-test was used. If the data did not show a normal distribution pattern, Wilcoxon signed-rank test was used. Time in minutes was presented as mean (±SD). Multiple linear regression models using Stata v. 6.0 software (Stata Corporation, College Station, Texas, USA) were used to show whether confounding factors such as age, sex and diagnosis had an influence on the result. Likelihood ratio tests were used to compare the different models, and finally, the best model with the fewest possible parameters was obtained.
A p value <0.05 (two-sided) was considered to be statistical significant.
Results
Only patients from the communities of Bülach, Bachenbülach, Winkel, Höri and Hochfelden were included in the analysis. A total of 770 patients contacted the GP on call in a doctor’s practice during Thursdays and weekends, between October 2006 and December 2006. During the same time interval, 694 patients living in the five communities cited above were seen at the emergency ward of the regional hospital of Bülach from Monday to Sunday. 231 patients were seen at the hospital on Thursdays and weekends. At this time interval, the population of these five communities was estimated to be 27 088.
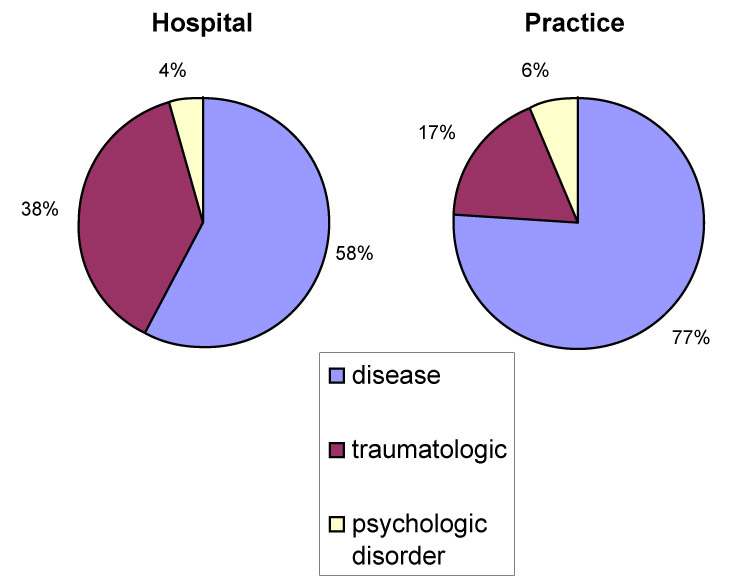
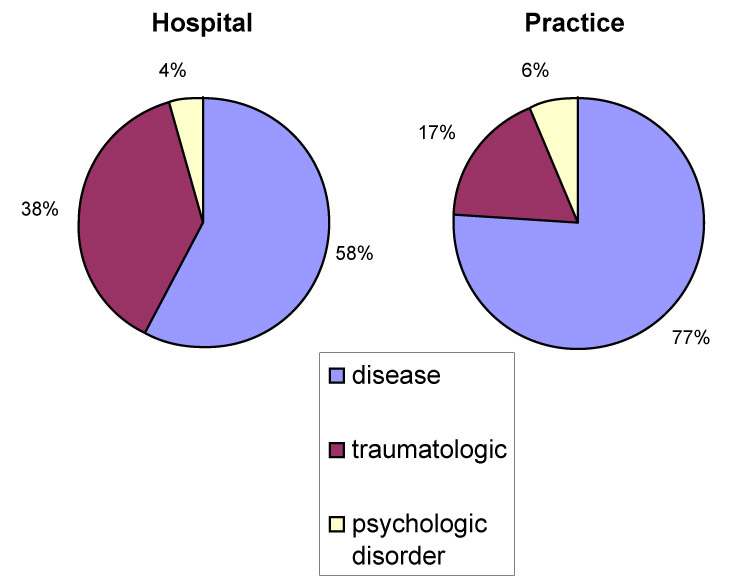
Figure 3
Distribution of patients seen for an emergency in the diagnosis categories of psychological disorder, traumatological disorder and medical disease. There was a difference in traumatological reasons for consultations between hospital and general practice.
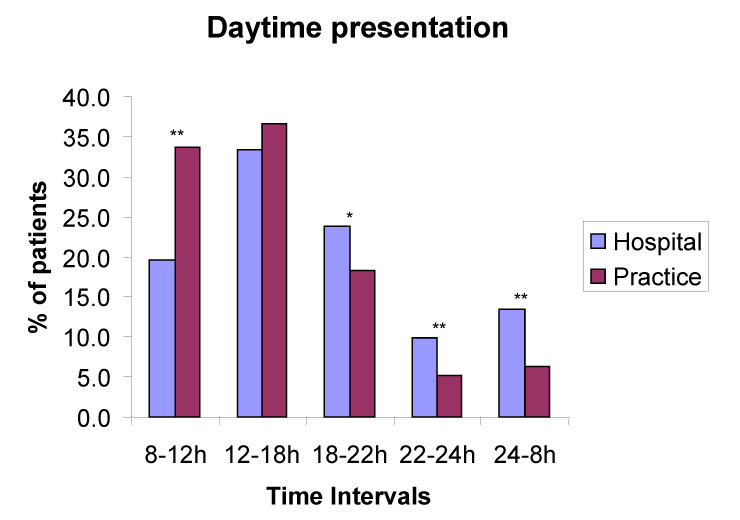
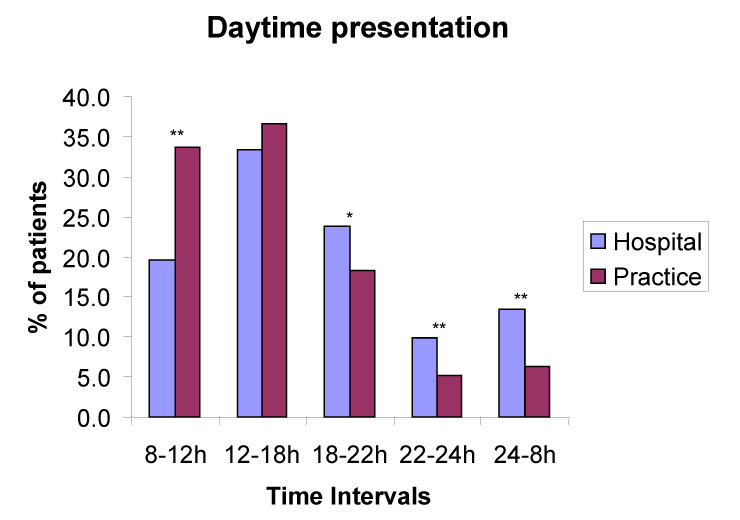
Figure 4
Relative distribution of patients seen for an emergency at different time intervals in percentages; comparison between hospital and general practice. *p <0.01; ***p <0.01.
Epidemiological data
A total of 770 patient contacts were registered by the practitioners on call in their practices, and in the same time, 231 patient contacts were registered in the hospital. From these 1001 patients, 96 patients needed hospitalisation or hospital diagnostic procedures, 32 patients were seen by the practitioners and sent to a hospital (patients were not sent to Bülach hospital only), and 64 hospitalised patients were only seen by the hospital staff. The epidemiological data are presented in table 1. Looking at the population attributed to these patients, the patient contact rate per day per 100 000 inhabitants was estimated to be 94.8, and the rate of patients who needed a hospital per 100 000 inhabitants per day was 9.1.
In table 2, patient and emergency characteristics are presented. Patients attended to at the hospital were older (the difference in age was statistically significant), consultation time was longer in the hospital (144.8 min vs. 19.6 min; p <0.0001) and patients in the hospital were more often estimated by attending physicians to have a real urgent case (92.7% vs. 68.8%, p <0.0001)
The diagnostic categories are demonstrated in table 3. Table 4 shows the multiple linear regression analysis table with consultation time as the dependent variable. The model explains 63% of the variability of consultation times. In this model, it could be shown that a GP practice as the place of consultation was strongly inversely correlated with consultation time (slope –2.005, p <0.0001; see table 4). The others, less important, but significant factors reducing consultation time were a gynaecologic reason for emergency consultation as a triage diagnosis, or a planned intervention in the hospital (planned control or investigation because of infertility) or in the GP practice (already taking prescribed drugs). If a simple linear regression with GP practice as a single factor was performed, 41.6% of the variation of the consultation time was explained by this factor, which emphasises the importance of this single factor inversely associated to consultation time.
As expected from the literature [10], ENT cases were common in our survey in CP-locations: 15.4% of all emergency consultations. Consultation time in all ENT cases comparing hospital and practice is shown in figure 1. A big difference in consultation time was noted between hospital consultations (144.3 ± 22.7) and consultations in a GP's practice (16.6 ± 0.9 min), and the difference was statistically significant (p <0.0001, Wilcoxon signed-rank). Figure 2 shows patient contacts, categorised in different age groups in percentages of the total hospital-attended patients and practice-attended patients. There was a difference in the paediatric population: 29.0% of patients attended by the primary care doctors are between 0 and 10 years old, compared to only 6.9% of patients in the hospital (p <0.0001 Chi2). Adolescents and younger adults, and patients of an older age (60–80 years old people) were seen more often in the hospital, whereas the geriatric population (>80 years) was seen more often by the GP on call. Figure 3 shows a distribution of raw diagnostic categories of psychological reasons, medical disease or traumatological disorders between hospital and doctor’s practice, respectively: Patients with traumatological reasons were more often attended at the hospital first, whereas patients with a non-surgical medical problem were attended more often by general practitioners. Figure 4 shows differences in presentation time during the day between hospital and general practice: During the daytime, more patients were seen by the practitioner on call than in the hospital, whereas after 6pm to 8am the next morning, more people were attended to in the emergency ward than by the general practitioner on call. 25.5% of patients seen at the hospital’s emergency department were hospitalised, compared to only 6.6% seen by GP’s.
| Table 1 |
| Total consultations |
1001 |
| Catchment area |
27088 |
| Consultations per day per 100 000 inhabitants |
94.8 |
| Total consultations by GP’s |
683 |
| Total hospital consultations |
318 |
| Emergencies seen by GP’s per 100 000 inhabitants per day |
64.7 |
| Hospital emergencies per 100 000 inhabitants per day |
30.1 |
| Total hospitalisations |
96 |
| Hospitalisations, requested by GP’s |
32 |
| Hospitalisations per 100 000 inhabitants per day |
9.1 |
| Table 2: Patient and emergency care characteristics, differentiated by GP and hospital cases, and statistical significance (continuous data: wilcoxon, for sex and urgency chi2-test). Data are presented as means and standard deviations (SD) if they are continuous and in numbers and percentages, if they are binary, respectively. |
| |
Hospital
|
Practice (GP)
|
p
|
| Age [years, SD] |
41.2 ± 22.8 |
32.6 ± 26.3 |
<0.0001 |
| Sex [female, (%)] |
372 (53.6) |
418 (54.9) |
0.61 |
| Consultation time [min, SD] |
144.8 ± 106.5 |
19.6 ± 17.6 |
<0.0001 |
| Urgent [yes, (%)] |
643 (92.7) |
544 (68.8) |
<0.0001 |
| Table 3: Estimation diagnoses of patients. |
|
Triage diagnosis
|
Hospital
|
Practice
|
|
|
n (%)
|
n (%)
|
| Traumatologic origin |
221 (31.8) |
112 (14.2) |
| Urology |
11 (1.6) |
13 (1.6) |
| Gynaecology |
24 (3.5) |
4 (0.5) |
| Rheumatology |
23 (3.3) |
64 (8.1) |
| Infections |
35 (5.0) |
149 (18.8) |
| Neurology |
19 (2.7) |
37 (4.7) |
| ENT |
27 (3.9) |
122 (15.4) |
| Allergies, dermatology |
29 (4.2) |
7 (0.9) |
| Thoracic pain |
36 (5.2) |
71 (9.0) |
| GI problems |
61 (8.8) |
75 (9.5) |
| Psychosomatic problems |
28 (4.0) |
47 (5.9) |
| Oncology, coagulation disorders |
9 (1.3) |
2 (0.3) |
| Ophthalmology |
1 (0.1) |
16 (2.0) |
| Other health services |
54 (7.8) |
14 (1.8) |
| Death assurance |
0 (0) |
3 (0.4) |
| Not known |
116 (16.7) |
55 (7.0) |
| Total |
694 |
791 |
| Table 4: Multiple regression analysis with logarithmic values, dependent variable consultation/waiting time of ENT cases only. The model explains 63% of the variability (R2 0.63). Slope β: slope of the regression; 95% CI: 95% confidence interval of the regression’s slope. Non significant variables were not included in the table and were: sex (p = 0.95) and estimation of emergency (p = 0.84). |
|
Factors
|
Observation numbers
|
Slope β (95% CI)
|
p value
|
| Consultation GP |
136 |
–2.005 (–2.281 – –1.729) |
<0.0001 |
| Age |
136 |
0.006 (0.001–0.012) |
0.021 |
| β0 |
136 |
6.545 (6.011–7.079) |
<0.0001 |
Discussion
This study demonstrates the epidemiology of patients looking for emergency primary care at the hospital and with a local GP. Due to the cross-sectional design of the study, only associations can be made from this data.
The presented data are the first population-based data of Switzerland concerning patients utilising emergency primary care services either performed by the general practitioner on call or by the hospital of the same region. As the data were taken at the same time, and because of the association of this data to the census data of that time, the obtained rates of 94.8 patient contacts per 100 000 inhabitants and the hospitalisation rate of 9.1 patients per 100 000 inhabitants seem to be reliable and valid, and are important information for planning the emergency primary care health system in Switzerland.
Furthermore, this study provides important data about emergency consultations: Children and geriatric patients seem to use health services provided by a general practitioner more often than going to an emergency ward of a hospital. The reason that children are more often seen by general practitioners in the region of Bülach seems to have a local reason, as the hospital does not offer a paediatric emergency primary care consultation service. On the other side, paediatricians do provide emergency services with general practitioners. In general, geriatric patients seem to consult out-of hospital services more often, which was also seen in a recently report from Norway [11]. An important finding of this study is the fact that patients at the hospital had a mean waiting and consultation time which was more than 8 times longer than the consultation time of a general practitioner on call. For this comparison, we only presented the data from patients who had a problem with their throat, nose or ears and who were not hospitalised (hospital) and were not sent by a GP to the hospital. A general practitioner who reported a case having a lot of consultations by different hospital physicians for cerumen obturans at an emergency ward in a hospital [12] gave us the idea to compare the management of ENT patients at the hospital and at a GP’s site. What could be the reason for this huge difference? An important point, leading to an overestimation of the difference was the fact that at the hospital the total time was measured, whereas for the patients at the general practitioners only consultation time was registered and not the time patients had to wait for attendance. Even if the time of consultation is subtracted from the total waiting time at the hospital, it is not likely that patients at a general practitioner’s office would wait so long for attendance. A possible reason for this difference could be that patients in emergency wards are treated according to the urgency of the medical problem they have, which leads to long waiting times for persons with minor problems, such as this examined group. Another possible reason might be the fact that patients contacting the GP by phone receive a timepoint to present themselves at the location, whereas at the hospital, first contact is often not announced by phone (walk-in). The lower hospitalisation rate of patients seen by GP’s compared to patients seen at the hospital indicates that patients presented at the hospital had a more severe health problem than patients attended by GP’s. It has to be mentioned that patients attended in the hospital are seen mostly by younger doctors who do not have as much experience as a general practitioner has. Therefore they need the senior staff to make a decision of treatment which takes more time. In addition, the lack of experience may lead to more use of laboratory analyses than a GP would use. There is indirect evidence for this last point mentioned: it has been shown that a senior emergency doctor put in the triage process in the emergency ward at a hospital can reduce the waiting time from 36 to 19 minutes [13]. Finally, the lab analysis of a GP might need a shorter time than a lab analysis in the hospital and some analyses performed in the hospital are more time consuming (such as troponin). All these factors may lead to a higher consultation and waiting time for patients attended at the hospital directly. Whatever the reason is, the data indicate that patients seen with health problems first by a GP in an emergency situation are probably treated in a more rapid way than with the classical hospital structures, which are made to treat major medical problems, and are not equipped to treat minor medical problems. In addition, the data confirm that ENT problems in primary care are a frequent health problem as mentioned by Hannaford et al. [10]. In contrast to this study, Hannaford’s data show general epidemiology of ENT problems in primary care in UK, showing a prevalence of 32.6% per year. This number is confirmed in a retrospective study from Spain, which estimated a prevalence of ENT problems of 34.6% per year [14]. The current study which shows a prevalence of 2.2% per year is not comparable to both above mentioned studies: our investigation describes only patients looking for emergency primary care and not all patients visiting a GP with ENT problems as both previously mentioned studies. Another explanation may be a different health care system between Switzerland – which still provides at the moment unrestricted (parallel) access to primary and secondary care services – and Spain and the UK, respectively, where primary care has a central referral (gatekeeping) role [15]. Comparing the contact rate at a hospital emergency department of 159 patients per 1000 inhabitants per 3 months with ENT problems in the UK [10], the contact rate of 100 patients per 1000 inhabitants per 3 months in our study appears lower. The difference might indicate that accessibility to primary care in Scotland might be reduced compared with German speaking Switzerland, and there is evidence supporting this theory in several studies [16, 17]. In the last years, hospitals in Switzerland have tried to organise their emergency service by putting a practice-like organisation besides the hospital together with general practitioners. The current study does not give an answer regarding whether this is the right way or not to go into the future, but it provides data which may be fundamental to reorganise the ambulatory emergency service. The current data show that per 100 000 inhabitants, it seems to be reasonable to plan 3 units of GPs giving a health service to the population, leading to approximately 30 patient contacts per unit. One Primary Care emergency unit per 30 000 inhabitants under guidance of general practitioners on weekend and nights could replace the traditional Swiss emergency care system using general practitioners with their own practice giving a 24-hour service 7 days a week. These units would not replace hospital emergency wards, but they could replace the traditional GP emergency service.
Another point is that the health system and the government should motivate young students to choose the specialty of general practitioner, which in fact seems not to be the case. Salaries of general practitioners have decreased dramatically in the past years leading to a lower motivation of students taking this career, and in a recently published report, only 10% of medical students at the university of Basel would take the future career of a general practitioner [18] – in fact – the situation in our emergency health system will aggravate.
What are the weaknesses of our study? Firstly, it is a cross-sectional study and because of that any predictions on the outcome cannot be made. Secondly, we did not consider the income of the patients analysed and therefore, the data do not give any information about socioeconomic gradients and the influence of this factor on the consumption of emergency health care. Thirdly, as the contact time between medical doctors and patients in the hospital were not available, total time at the emergency ward was taken as consultation time. This might lead to a considerable overestimation of the presented effects concerning clinical performance. Of course, a direct comparison between hospital waiting and consultation time and GP consultation time is difficult and is definitely a limitation of this study.
In conclusion, our study gives information regarding how many patients are looking for emergency professional help per population. These data are important to consider for planning the future of Swiss emergency health care. In addition, the data show that general practitioners are less time consuming for patients looking for adequate health care immediately. The data generate the hypothesis that general practitioners might be more time-efficient than the classical hospital pathway of patients looking for emergency primary care. The latter has to be confirmed in prospective studies.
Correspondence:
Jean-Pierre Gutzwiller MD MPH
Internal Medicine & Gastroenterology
CH-4800 Zofingen
Switzerland
jean-pierre.gutzwiller@unibas.ch
References
1 Bernstein AB, Hing E, Moss AJ, Allen KF, Siller AB, Tiggle RB. Health care in America: trends in utilization [DHHS Publication No. 2004-1031]. Hyattsville, MD: National Center of Health Statistics; 2003.
2 Derlet R, Richard J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151–5.
3 Santos-Eggimann B. Increasing use of the emergency department in a Swiss hospital: observational study based on measures of the severity of cases. BMJ. 2002;324:1186–7.
4 Flaig C, Zehnder K, Zürcher H, Eichenberger P, Frei C, Gegeckas A, et al. Selbsteinweisungen ins Spital. PrimaryCare. 2002;2:280–3.
5 Schwappach DLB, Blaudszun A, Conen D, Ebner H, Eichler K, Hochreutener MA. “Emerge”: benchmarking of clinical performance and patients’ experiences with emergency care in Switzerland. International Journal for Quality in Health Care 2003;15(6): pp. 473–85.
6 Arnet B, von Below G. Organisation des ambulanten ärztlichen Notfalldienstes in der Schweiz. 2002 http://www.sggp.ch/schriften/liste/band81.cfm
7 Hugentobler W. Kostenvergleich der ambulanten Notfallversorgung in der hausärztlichen Praxis mit den Notfallstationen der Spitäler. PrimaryCare. 2006;6:586–9.
8 Marty F, Meyer R, Lüscher S, Gnädinger M, Kissling B. Dringliche Konsultationen/Notfälle beim Hausarzt – eine Pilotstudie. PrimaryCare. 2006;6:345–7.
9 Statistisches Amt des Kantons Zürich, Blicherweg 5, 8090 Zürich. http://www.statistik.zh.ch
10 Hannaford PC, Simpson JA, Bisset AF, Davis A, McKerrow W, Mills R. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland. Fam Pract. 2005;22:227–33.
11 Zakariassen E, Burman RA, Hunskaar S. The epidemiology of medical emergency contacts outside hospitals in Norway – a prospective population based study. Scand J Trauma Resusc Emerg Med. 2010;18:9.
12 Christen ST. Cerumen obturans – 500 Franken. Schweiz. Ärztezeitung. 2006;87(8):301.
13 Travers JP, Lee FCY. Avoiding prolonged waiting time during busy periods in the emergency department: is there a role for the senior emergency physician in triage? Eur J Emerg Med. 2006;13:342–8.
14 Sicras-Mainar A, Pané-Mena O, Martínez-Ruíz T, Fernández-Roure JL, Prats-Sánchez J, Santafé L, et al. Utilización de los grupos clínicos ajustados en un centro de atención primaria español: estudio retrospectivo de base poblacional. Rev Panam Salud Publica. 2010;27:49–55.
15 Hannaford PC, Smith BH, Elliott AM. Primary care epidemiology: its scope and purpose. Fam Pract. 2006;23:1–7.
16 McCusker J, Karp I, Cardin S, Durand P, Morin J. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med. 2003;10:1362–70.
17 Ionescu-Ittu R, McCusker J, Ciampi A, Vadeboncoeur AM, Roberge D, Larouche D, et al. Continuity of primary care and emergency department utilization among elderly people. CMAJ. 2007;177:1362–8.
18 Tschudi P. Der Hausarzt – Spielball der Patienten und der Gesundheitspolitik? PrimaryCare. 2009;9:158–62.