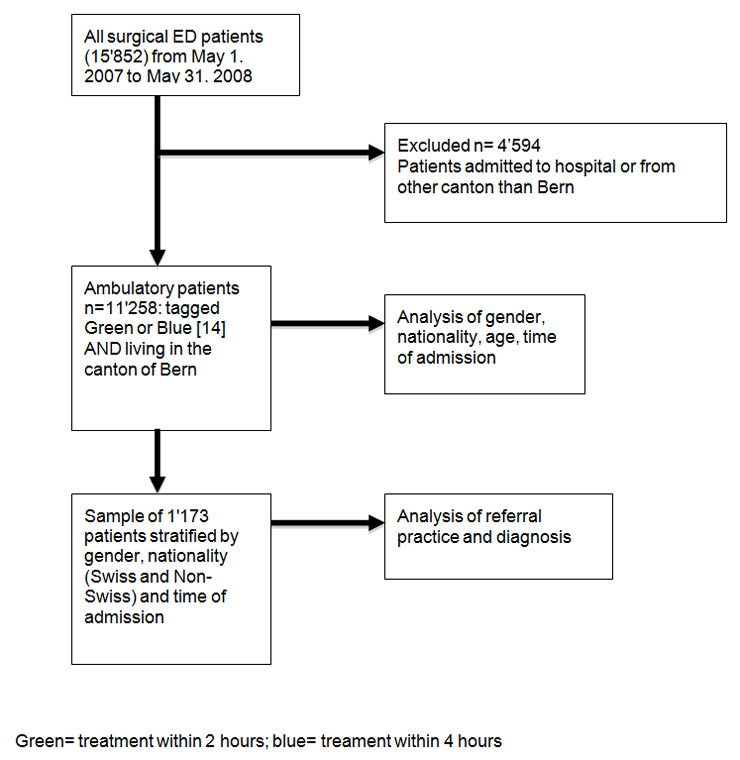
Figure 1
Study design.
DOI: https://doi.org/10.4414/smw.2010.13089
An analysis of 11258 patients
Emergency department (ED) crowding is an increasingly significant national and international problem [1–5]. Many studies have described characteristics of patients admitted to EDs in different countries, including socioeconomic factors [1–5]. Overcrowding has many potential detrimental effects, e.g., diversion of ambulances, frustration of patients and ED personnel, decreased patient satisfaction [6], higher costs [7, 8], and, most importantly, greater risk of poor outcome [8, 9]. Furthermore overcrowding may corrupt ED staff training for major trauma, an important function of EDs in medical education [10].
Overcrowding is partially caused by the growing number of visits by so called “walk-in patients” with minor problems who could easily be seen by a general practitioner (GP). Previous studies have shown that an increasing number of patients use the ED as their primary health-care provider [11, 12]. Approaches designed to optimise capacity planning and patient pathways using simulation tools are a possible way to deal with internal problems of ED organisation and thus could help in using ED resources more efficiently [13]. But even the most efficient ED may face overcrowding that cannot be optimised internally but must be addressed in a more general way by guiding patients to primary care by GPs instead of ED services.
The aim of our study was to assess the relationship between nationality, gender and age and the use of our health services among patients visiting an urban university hospital ED.
In our study we intended to assess the distribution of case load with non-urgent patients at our ED. The case load has a direct effect on the organisation of ED staff working shifts.
Our study was conducted from May 1, 2007 to May 31, 2008 in an inner city surgical trauma and emergency unit with approximately 15000 annual surgical ED visits. The emergency unit at the Inselspital, University Hospital Bern, Switzerland, is the only Level 1 accident and emergency unit in this area providing service for all social classes and insurance groups.
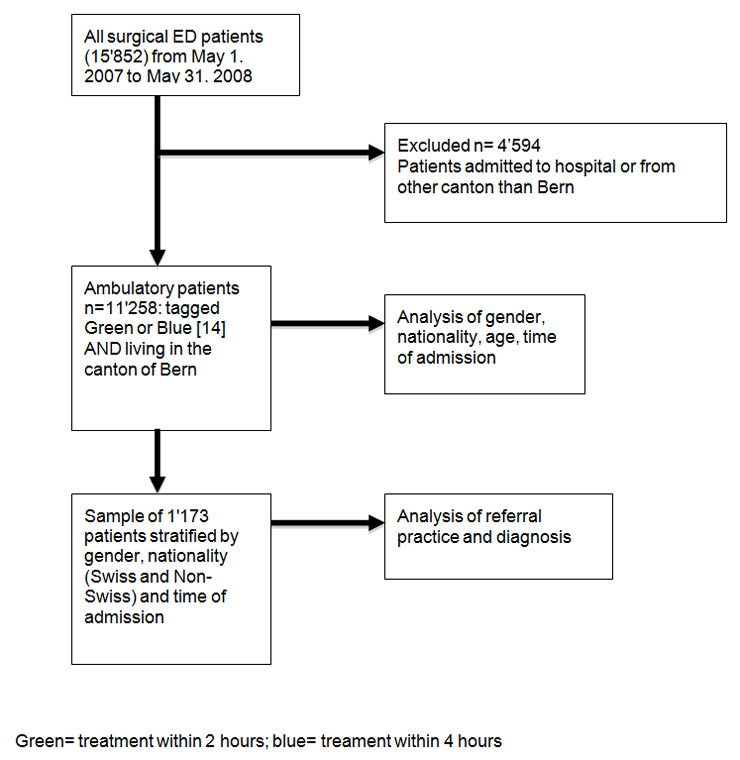
Figure 1
Study design.
Patients in our ED are routinely triaged using an abbreviated version of the Manchester Triage System [14].
This triage system defines the possible delay of treatment for patients presenting to an ED. Patients tagged green or blue usually need treatment within 2 to 4 hours (table 1).
The data were collected prospectively using our SAP patient database, in which all ED visits are registered. Data on insurance status, employment, nationality based on identity card, referring doctor and patient’s GP are included in our registry.
Out of all admitted patients we included patients for further analysis who were tagged green or blue according to the Manchester triage system [14] and lived in the canton of Bern. The treatment of these patients can be delayed by 2 to 4 hours. Patients admitted to hospital or from outside the canton of Bern were excluded.
A stratified sample based on gender, nationality and time of admission, with a total of 1173 patients, was taken for further analysis. For these patients we collected the additional data from our emergency room patient administration software Qualicare (Meierhofer AG, München, Germany). For a detailed diagram of the patient selection and analysis process, see figure 1.
Time of admission was split into three major time frames, adapted to the hospital personnel’s working shifts. The time frames were from 0:00 am to 7:00 am, 7:00 am to 7:00 pm, and 7:00 pm to 12:00 pm. We defined weekend hours as being from Friday 7:00 pm to Monday 7:00 am. We defined late evening to early morning hours (e.g., 7:00 pm to 7:00 am) and weekends as unsocial hours due to reduced hospital staff and unavailability of certain services in the hospital at these hours. We defined hours from 7:00 am to 7:00 pm during weekdays as social hours.
We defined hours from 7:00 pm to 12:00 pm as late evening hours and hours from 0:00 am to 7:00 am as early morning hours.
Patients were classified as Swiss and non-Swiss citizens. The non-Swiss citizens were further grouped into European Union, African, Balkan and other nationality. Nationality was recorded on the basis of identity card or passport.
Continuous data with a normal distribution were expressed as mean and standard deviation or as median and range, and dichotomous data were presented as frequencies and percentages. Data were analysed using Student’s t test when normally distributed and the Mann–Whitney U test when not normally distributed. Dichotomous variables were analysed by the χ2 test or Fisher’s exact test. A 2–sided P<0.050 was considered statistically significant. All statistical analyses were performed using SPSS® 17.0 (SPSS; Chicago, Illinois, USA).
| Table 1 Patient treatment priorities according to the Manchester Triage System [14]. | ||
| Urgency | Triage colour | Maximum time to treatment |
| Immediate | Red | Immediately |
| Very urgent | Orange | Within 10 minutes |
| Urgent | Yellow | Within 1 hour |
| Standard | Green | Within 2 hours |
| Non-urgent | Blue | Within 4 hours |
In all, 6955 male (61.8%) and 4303 female (38.2%) patients were included in our study (total of 11258 patients). Of all visits 2948 (26.18%) were by foreign nationals, a percentage which is significantly higher than the non-Swiss population of Bern (28 662; 22.1%, p <0.001) [15, 16]. Out of all patients, 1124 (9.99%) were from EU countries, 429 (3.81%) were from Balkan countries, 228 (2.03%) from African and 1164 (10.35%) from other countries.
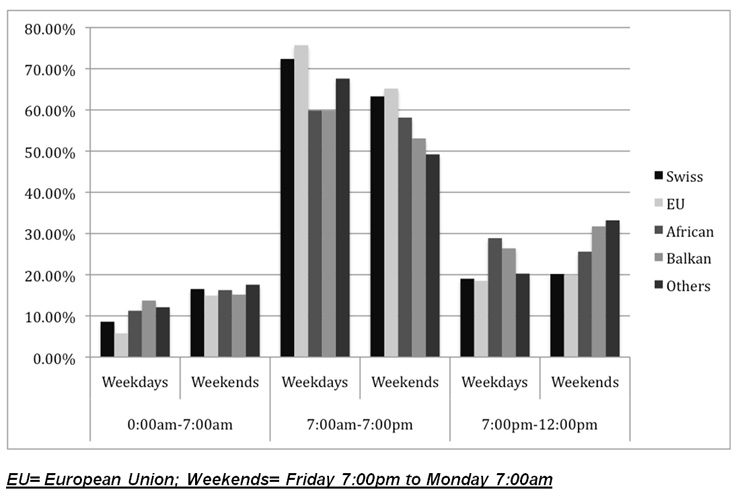
Figure 2
Distribution of patient admissions by time period and nationality on weekdays and weekends in percentages.
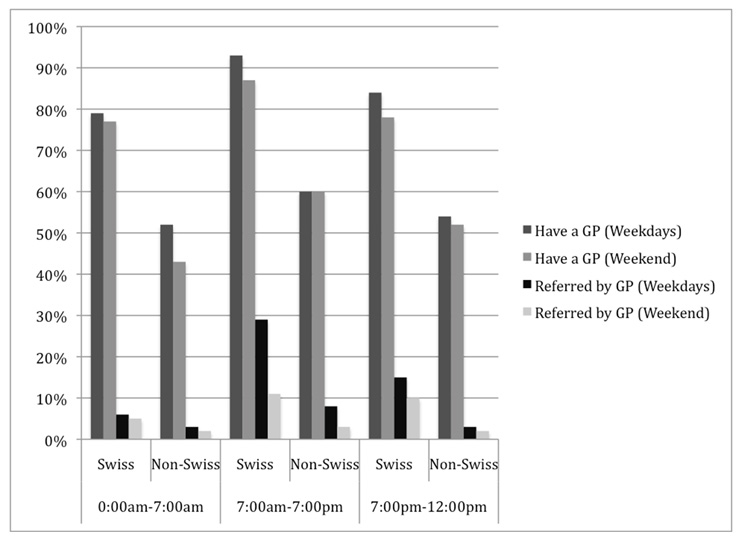
Figure 3
Patients having a general practitioner (GP) and patients being referred by a GP for Swiss vs. Non-Swiss patients on weekdays and weekends.
Non-Swiss male patients were significantly younger than Swiss male patients (median age 35 [range 2–89] years versus 45 [1–98] years, p <0.0001). Non-Swiss female patients were younger than Swiss female patients (32 [1–99] years versus 37 [3–95] years, p <0.0001). Detailed demographic data are shown in table 2. The distribution of all patients by time of admission for weekends and weekdays, reflecting the spread of the caseload of our ED on weekends and weekdays, is shown in figure 2.
Swiss patients significantly more often presented during social hours compared to non-Swiss nationals (69.4% versus 63.2%, p <0.0001). In the groups of non-Swiss nationals, patients of the European Union showed almost the same distribution with respect to social and unsocial hours as Swiss nationals. Patients from Balkan and African countries visited the ED significantly more often during unsocial hours (42.4% and 40.8% versus 30.6% for Swiss nationals, p <0.0001). At weekends in particular, they showed a higher rate of admissions during the late evening and early morning hours (fig. 2).
There are differences in the behaviour of female and male patients: foreign male patients are significantly overrepresented between 7:00 pm and 12:00 pm compared to Swiss male patients (21.6% versus 13.4%, p <0.0001).
Swiss male patients presented significantly more often between 7:00 am and 7:00 pm than non-Swiss male patients (73% versus 65%, p <0.0001) and significantly less often during the period from 7:00 pm to 12:00 pm (13.4% versus 22%, p <0.0001). In the period between 0:00 am and 7:00am there was no difference between the two groups (13% for both, p = 0.5).
Swiss female patients presented significantly more often during the time between 7:00 am and 7:00 pm compared to non-Swiss female patients (72% versus 65%, p <0.0001). Non-Swiss female patients presented significantly more often between 7:00 pm and 12:00 pm (25% versus 21%, p <0.0001) and 0:00 am and 7:00 am compared to Swiss female patients (10% versus 7%, p <0.0001).
Neither Swiss nor non-Swiss female patients visited the ED more frequently during weekends than male patients (p = 0.74).
From all Swiss patients 67% referred themselves (walk-in patients) without a previous GP visit, compared to 79% self-referrals among foreigners (402/598 Swiss versus 454/575 non-Swiss patients, p <0.0001).
83% of Swiss patients visited a GP regularly, compared with 57% of non-Swiss patients (498/598 Swiss versus 331/575 non-Swiss, p <0.0001). Swiss citizens were significantly more often admitted by their GP than non-Swiss patients (p <0.0001 for all time periods; fig. 3). There was no significant difference between Swiss and non-Swiss patients in terms of admission due to trauma or other reasons (p = 0.31). Most patients included in our stratified sample presented minor surgical problems such as bruises, contusions or wounds possibly needing suture in the ED, conservatively treated fractures or otorhinolaryngological problems. Table 2 shows the most common diagnoses in these patients.
| Table 2 General demographic patient characteristics. | ||||
| Nationalities | Male N (%) | Female N (%) | Age male (median, range) | Age female (median, range) |
| Swiss | 5074 (45%) | 3239 (28.8%) | 45 (1–98) | 37 (3–95) |
| EU | 716 (6.4%) | 408 (3.6%) | 39 (2–89) | 32 (1–99) |
| Balkan | 304 (2.7%) | 123 (1.1%) | 33 (2–76) | 36 (4–71) |
| African | 156 (1.4%) | 69 (0.6%) | 33 (6–83) | 33 (6–76) |
| Others (e.g. USA, South America, Asia, etc.) | 705 (6.3%) | 464 (4.1%) | 34 (3–86) | 35 (3–87) |
| Table 3 Clinical diagnosis of sample-patients (n = 1173). | ||
| Main diagnosis | Number of patients | Relative rate (%) |
| Bruises, contusions | 118 | 10.1 |
| Unspecific abdominal pain | 72 | 6.1 |
| Otitis, auditory canal diseases | 69 | 5.9 |
| Contused wounds, lacerations | 59 | 5.0 |
| Cutting wounds | 57 | 4.9 |
| Conservatively treated fractures | 54 | 4.6 |
| Other orthopaedic diseases | 53 | 4.5 |
| Mild traumatic brain injury (GCS 14–15) | 51 | 4.3 |
| Other urological problems | 49 | 4.2 |
| Superficial infection or abcesses | 45 | 3.8 |
| Epistaxis | 39 | 3.3 |
| Ankle distorsion | 38 | 3.2 |
| Violence related injury (minor) | 36 | 3.1 |
| Urinary infection | 30 | 2.6 |
| Anal and perianal disease | 18 | 1.5 |
| Non-dislocated nasal fractures | 18 | 1.5 |
| Non-specific viral infection | 11 | 0.9 |
| Other diagnosis (e.g., tick bites, pharyngitis, foreign body, etc) | 314 | 30.5 |
| Total number of patients | 1173 | 100 |
| GCS = Glasgow Coma Scale | ||
Our results show that nationality is significantly associated with greater use of ED services for non-urgent problems. Patients from African and Balkan countries in particular use the ED more frequently during the early morning, late evening and at weekends compared to Swiss nationals.
The usual slogan that patients should seek the assistance of GPs first before consuming rare and expensive hospital resources may not operate – simply because many patients do not have a GP. Several explanations are conceivable. One may be the lack of GPs of foreign origin who would be more sensitive to cultural differences [17].
To test this hypothesis we searched the register of GPs in the city of Bern and found a total of 128 registered GPs. Of these 128 GPs, only 7 apparently had non-Swiss surnames, accounting for a rate of 5.5%, compared to 94.5% with a Swiss family name. Compared to the total non-Swiss population in Switzerland and in Bern, which is 22.1%, this rate is very low. We admit that this method of addressing GPs by nationality is certainly very limited, since foreign GPs may have Swiss names and vice versa, and interpret this result only in terms of showing a possible tendency that might affect GP care.
Other reasons may be linked to cultural attitudes towards public services or the fear of leaving one’s workplace for medical visits. Clinical and policy efforts must erect bridges to GP care for these patients, since in the long term GP care provides better and more cost effective care for patients with minor complaints [8, 18, 19]. Furthermore, GPs can establish a long term relationship with patients, resulting in better knowledge of sociocultural and individual habits and needs. This leads to a higher patient satisfaction, better outcomes for medical health issues and fewer hospitalisations [20, 21].
It is clear that GPs, depending on their equipment and personal experience, cannot handle all types of minor surgical problems. As GPs in Switzerland are usually well equipped in their practice, we expect that most of those minor injuries (bruises, contusions, contused and cutting wounds, ORL-problems, urinary tract infections or other infections) can be easily diagnosed and treated adequately without the need for highly specialised equipment or training.
As foreign nationals admitted to our ED were significantly younger compared to Swiss patients, age may play a role since younger patients tend to use the ED as a primary health care source instead of going to the GP. Lang et al. reported that people using the ED as their primary source of care were significantly younger, which is consistent with our results [11]. Junot Perron et al. showed that in Switzerland patients using a private practice instead of an university outpatient clinic were significantly older, had a better education and higher income than patients using a university outpatient clinic [22]. The patients favouring the GP for regular visits presented at the ED less often than patients preferring the outpatient clinic [22]. Althaus et al. reported that non-Swiss nationals living in Switzerland have more health problems than Swiss nationals and are of lower socio-economic status [22].
In our study we showed that non-Swiss patients visited the ED more often during unsocial hours, resulting in a relevant increase in workload during these hours. This trend can lead to even more frustration in the ED staff and increase waiting times for patients. The trend to visits during late evening or early morning or at weekends has been described in other countries as well [4]. The implication of these results is that staffing might be increased during these unsocial hours to ensure appropriate treatment for all patients visiting the ED. Future studies may address the personal case load and work load of ED staff in order to assess whether or not staffing in the ED is adequate during these high workload hours.
We admit that many patients who seem to have minor problems may still need hospital admission for adequate treatment. We therefore see the need for further prospective trials on this subject.
We would like to thank Dr. Rodney Yeates for language editing and Mr. Andy Schötzau for statistical advices.
1 Bianco A, Pileggi C, Angelillo IF. Non-urgent visits to a hospital emergency department in Italy. Public Health. 2003;117:250–5.
2 Lang T, Davido A, Diakite B, Agay E, Viel JF, Flicoteaux B. Non-urgent care in the hospital medical emergency department in France: how much and which health needs does it reflect? J Epidemiol Community Health. 1996;50:456–62.
3 Agouridakis P, Hatzakis K, Chatzimichali K, Psaromichalaki M, Askitopoulou H. Workload and case-mix in a Greek emergency department. Eur J Emerg Med. 2004;11:81–5.
4 Wallis LA, Twomey M. Workload and case mix in Cape Town emergency departments. S Afr Med J. 2007;97:1276–80.
5 Oktay C, Cete Y, Eray O, Pekdemir M, Gunerli A. Appropriateness of emergency department visits in a Turkish university hospital. Croat Med J. 2003;44(5):585–91.
6 Pines JM, Iyer S, Disbot M, Hollander JE, Shofer FS, Datner EM. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15(9):825–31.
7 Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994;12(3):265–6.
8 Campell MK, Silver RW, Hoch J, Ostbye T, Stewart M, Barnsley J, et al. Re-utilization outcomes and costs of minor acute illness treated at family physician offices, walk-in clinics, and emergency departements. Can Fam Physician. 2005;51:82–3.
9 Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184(5):208–12.
10 Saxer T, Duperrex O, Vermeulen B, Vu Nu V. Emergency medicine training: a prospective, comparative study of an undergraduate clinical clerkship and army program. Swiss Med Wkly. 2009;139(29–30):423–9.
11 Lang T, Davido A, Diakite B, Agay E, Viel JF, Flicoteaux B. Using the hospital emergency department as a regular source of care. Eur J Epidemiol. 1997;13:223–8.
12 Backman AS, Blomqvist P, Lagerlund M, Carlsson-Holm E, Adami J. Characteristics of non-urgent patients. Scand J Prim Health Care. 2008;26:181– 7
13 Exadaktylos AK, Evangelopoulos DS, Wullschleger M, Bürki L, Zimmermann H. Strategic emergency department design: An approach to capacity planning in healthcare provision in overcrowded emergency rooms. Journal of Trauma Management & Outcomes. 2008;2:11.
14 Mackway-Jones K. Emergency triage. London: BMJ Publishing. 1997.
15 Ausländerinnen und Ausländer in der Schweiz, Bericht 2008. Bundesamt für Statistik, Eidgenössisches Departement des Inneren, Schweizerische Eidgenossenschaft 2008. http://www.bfs.admin.ch/bfs/portal/de/index/news/publikationen.html?publicationID=3403 (last access 05.27.2010) Ausländische Wohnbevölkerung nach Heimatstaat und Bewilligungsart Ende 2009. Statistikdienste der Stadt Bern, Schweiz 2009. http://www.bern.ch/leben_in_bern/stadt/statistik/bevoelkerung/jaehrlich/2110bevauslnatiobew.pdf (last access 05.27.2010)
16 Berger JT. The influence of physicians’ demographic characteristics and their patients’ demographic characteristics on physician practice: implications for education and research. Acad Med. 2008;83(1):100–5.
17 Mehrota A, Liu H, Adams J, Wang MC, Lave J, Thygeson M, et al. The cost and quality of care for three common illnesses at retail clinics compared to other medical settings. Ann Intern Med. 2009;151(5):321–8.
18 De Maeseneer JM, De Prins L, Gosset C, Heyerick J. Provider continuity in family medicine: does it make a difference for total health care costs? Ann Fam Med. 2003;1:144–8.
19 Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabetic Medicine. 2003;20:486–90.
20 Fan VS, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20:226–33.
21 Junot Perron N, Favrat B, Vannotti M. Patients who attend a private practice vs a university outpatient clinic: how do they differ? Swiss Med Wkly. 2004;134:730–7.
22 Althaus F, Paroz S, Renteria SC, Rossi I, Gehri M, Bodenmann P. Gesundheit von Ausländern in der Schweiz. Swiss Med Forum. 2010;10(4):59–64.
No funding; no competing interests.