Table 1
DOI: https://doi.org/10.4414/smw.2010.13056
In medicine, postgraduate trainees can generally aim for a broad range of different career paths. Some graduate students follow a traditional training in a clinical specialty aspiring to a career in private practice or in hospital. Some specialise in basic sciences and then they often pursue an academic career. Others will leave patient-centred medicine, and work in pharmaceutical companies, in medical informatics or in public health institutions. Depending on the chosen specialty or medical field, some career paths are predetermined, such as family medicine in private practice, and surgery and anaesthesiology mainly in hospitals. In Switzerland, postgraduate training is regulated and certified by the respective Swiss Society of a certain specialty and the Swiss Medical Association (FMH). There are no official limitations of how many medical school graduates get a residency post for further education in a certain specialty, as common practice in many countries [1–3]. However, in highly specialised and prestigious medical fields, such as cardiology, gastroenterology, ophthalmology, oto-rhino-laryngology or urology, the Swiss Specialty Societies limit the number of residency posts to control the number of qualified specialists.
To date there are several cohort studies on the specialty choice of young physicians [4–7]. However there are hardly any reports on the issue regarding at what stage of their postgraduate training the residents decide for a certain career path in medicine, what factors have an impact on the choice of a career path, and what variables are associated with a certain career path [7–8]. The present study aimed to address these issues. The following questions were investigated: (1) what career paths can be identified in the course of the physicians’ postgraduate training? (2) What factors have an influence on a person’s choice of a certain career path? (3) In what way are the career paths correlated with workload, career success and work-life balance aspirations?
The present study was part of an ongoing prospective survey of a cohort of graduates of the three medical schools in German-speaking Switzerland (Basel, Bern, and Zurich) (SwissMedCareer Study),which began in 2001 (T1) [9]. Seventy-one percent (n = 711) of all registered final-year students (N = 1004) in these three medical schools participated in the baseline assessment. Subjects were re-evaluated every two years. The present paper refers to the results of the assessments from T2 through to T5. At T1, the participants were still in medical school, while at T2 they had entered postgraduate training. From this time on they were working as residents, and they were asked at every assessment, which career path in medicine they aspired to have. The fifth assessment was conducted in 2009, seven years after graduation.
To ensure participants’ anonymity, the returned questionnaires were only identified by a code. The respondents sent their current addresses to an independent address-administration office, allowing for follow-up. The study was approved by the ethical committee of Zurich University.
The sample of the present studyconsisted of 358 physicians (197 females, 55%; 161 males, 45%) participating at any assessment from T2 to T5, and answering the question: What career path do you aspire to have? The mean age of the participants at T5 was 35.3 years (SD 2.1 years, range 33–49 years). Of the respondents, 307 (86%) lived in a stable partnership, of whom 181 are married. Of 307 partnerships, 113 (37%) were dual doctor couples. Seventy-two (36%) of the females, and 62 (38%) of the males had children at T5. To those physicians who did not participate at any assessment, we cannot refer in terms of their career path aspirations.
All instruments are self-assessment scales. In the following, the constructs measured by the instruments are described:
– Questions concerning socio-demographic data
– Workload (h/week)
– Specialty choice(primary care, internal medicine including all sub-specialties, surgical fields, anaesthesiology, gynaecology & obstetrics, paediatrics, psychiatry, other medical specialties such as ophthalmology, oto-rhino-laryngology, radiology, pathology etc.)
– Career aspired to have:not yet decided, medical practice, hospital medicine, academic medicine, other medicine-related fields (e.g., pharmaceutical companies, public health institutions, health administration, medical informatics)
– Personal Attributes Questionnaire, GE-PAQ, German Extended Personal Attributes Questionnaire [10], is a self-rating instrument for the assessment of gender-role orientation. It consists of 16 bipolar items (six-point Likert scale). The Instrumentality (PAQ-I) scale contains eight instrumental traits (e.g., “independent”, “decisive”) that are considered to be socially desirable to some degree in both sexes, but are stereotypically more characteristic of males. The Expressiveness (PAQ-E) scale contains eight items that describe socially desirable expressive, communal traits (e.g., “helpful”) that are stereotypically more characteristic of females.
– Occupational Self-Efficacy Expectation Questionnaire (Fragebogen zu beruflichen Selbstwirksamkeitserwartungen (BSW, 6 items, five-point Likert scale) [11]: The BSW questionnaire is a measure of a person’s general occupational self-efficacy expectations.
– Career Motivation Questionnaire(CMQ, seven-point Likert scale) [12] consists of 3 scales with 8 items each: Intrinsic Career Motivation CMQ-I (i.e. enjoyment of and interest in professional activities), Extrinsic Career Motivation CMQ-E (i.e. striving for promotion, income, prestige) and Extraprofessional Concerns CMQ-EC(i.e. prioritising family, convenient working hours, job security).
– Mentor-Protégé Relationships Questionnaire[13] (Likert scale 0–4) consists of five scales measuring different types of career-support. We used the Networking Scale(4 items) and the Support in career planning scale (3 items). These two scales describe crucial aspects of mentoring. Our data analyses show that the two scales are highly correlated (r = 0.71). We therefore combined them into one scale named ‘Mentoring-Experience Scale’, having a high Cronbach’s alpha = 0.93.
– Work-life Balance aspired to (5-point Likert scale) [14] investigates which of four different models of work-life balance (career orientation, balance of work and personal life, part-time orientation, three-phase orientation: work-family break-work) the participants want to realise within 5 years.
– Career Success Scale[15] is a measure of objective career steps consisting of 7 items addressing scientific activities (lectures at conferences, publications, collaborating in large research projects, research as main field, scholarships and grants; these are criteria corresponding to the requirements for tenure track).
– Subjective Assessment of Career Success [16] is a measure of one’s own career advancement compared to other cohort subjects (7-point Likert scale, 1 = less successful, 7 = more successful).
– Question on Satisfaction with Career Success[9] (7-point Likert scale, 1 = very unsatisfied, 7 = very satisfied) is a measure of a person’s satisfaction with his/her career success.
Cluster analysis: At any of the four assessments, physicians were surveyed on their future career path aspiration: They could answer this item in the questionnaires by choosing one of the five given categories “not yet decided”, “medical practice”, “hospital medicine”, “academic medicine”, “other medicine-related fields (e.g. pharmaceutical companies, public health institutions, health administration, medical informatics)”. Theses four variables (one per assessment) were entered in a two-step cluster analysis according to Bacher et al. [17–18]. This method is a sorting algorithm, producing a classification of subjects at most homogeneous clusters by a defined set of variables and creates distinct types (profiles) of subjects. The statistical parameters in the procedure are estimated with maximum-likelihood method and the number of clusters is determined by the ratio of distance measures [17].
The statistical analysis was performed with the SPSS 15 statistical software program. Descriptive data is presented in absolute frequencies, percentages, mean values and 95% confidence interval for means. Differences between the clusters in person-related characteristics, career motivation, mentoring experience, work-life balance, workload, career success, and satisfaction with career were analysed by multiple analyses of covariance, taking into account the correlations between these variables and controlling for gender as a covariate. Multivariate and univariate F-tests, controlled for gender, p-values, and partial Eta-square are reported as well as Bonferroni multiple comparisons between the clusters. Differences in gender, parenthood, and specialty choice were analysed with Chi-square tests. p-values lower than 0.05 were considered to be significant.
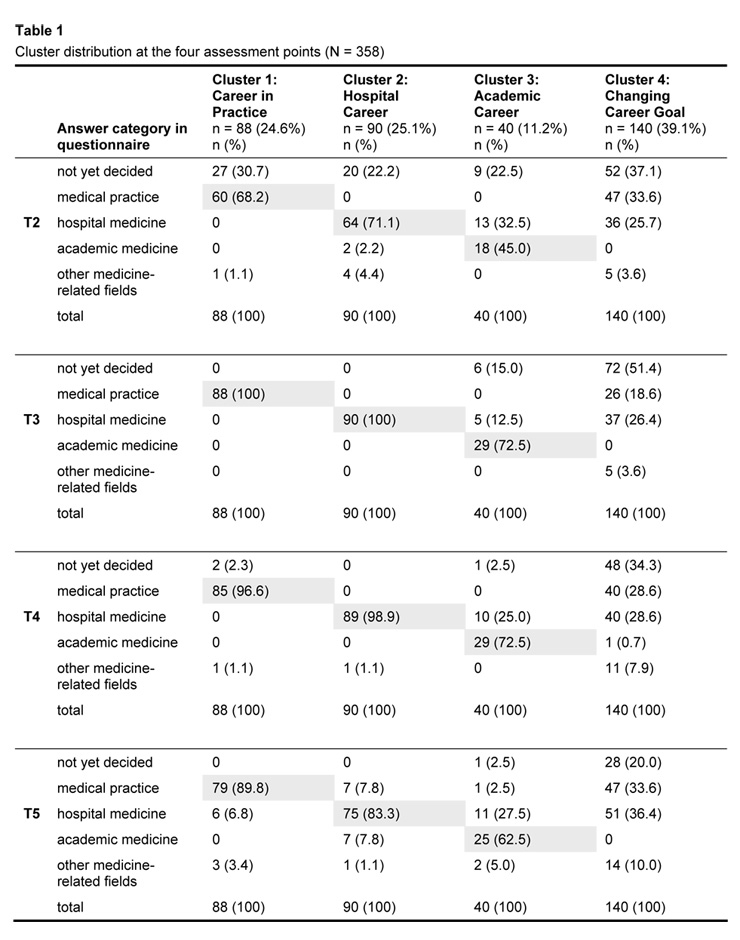
In a prospective career development study it was of interest whether specific career path aspirations can be identified in a cohort of postgraduate doctors. The cluster analysis revealed four career clusters which distinctly discriminate between each other. In table 1, the distribution of the four clusters in terms of career path aspired to over the four assessment points is listed.
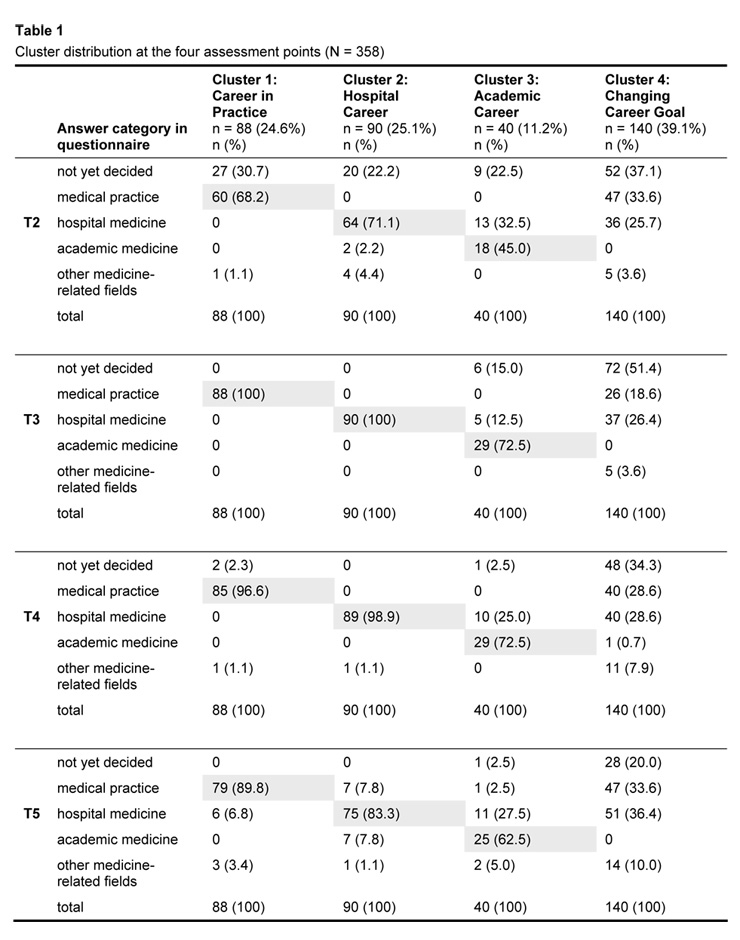
Table 1
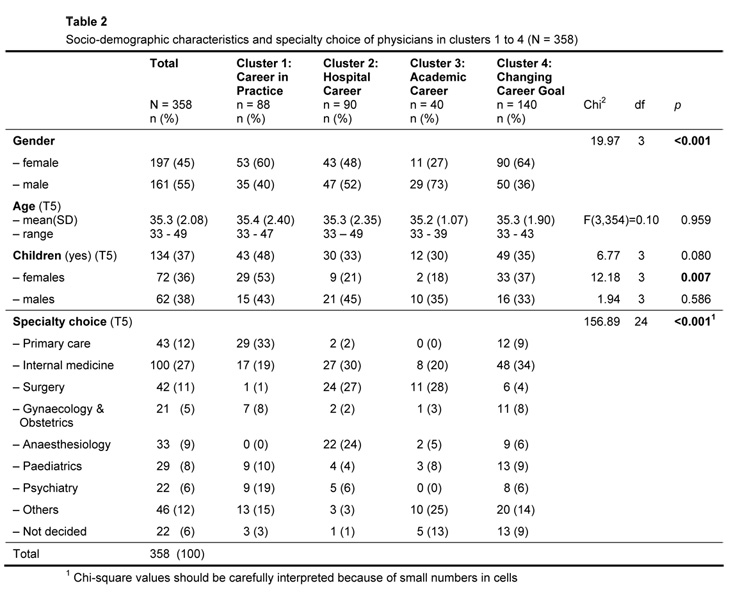
Table 2
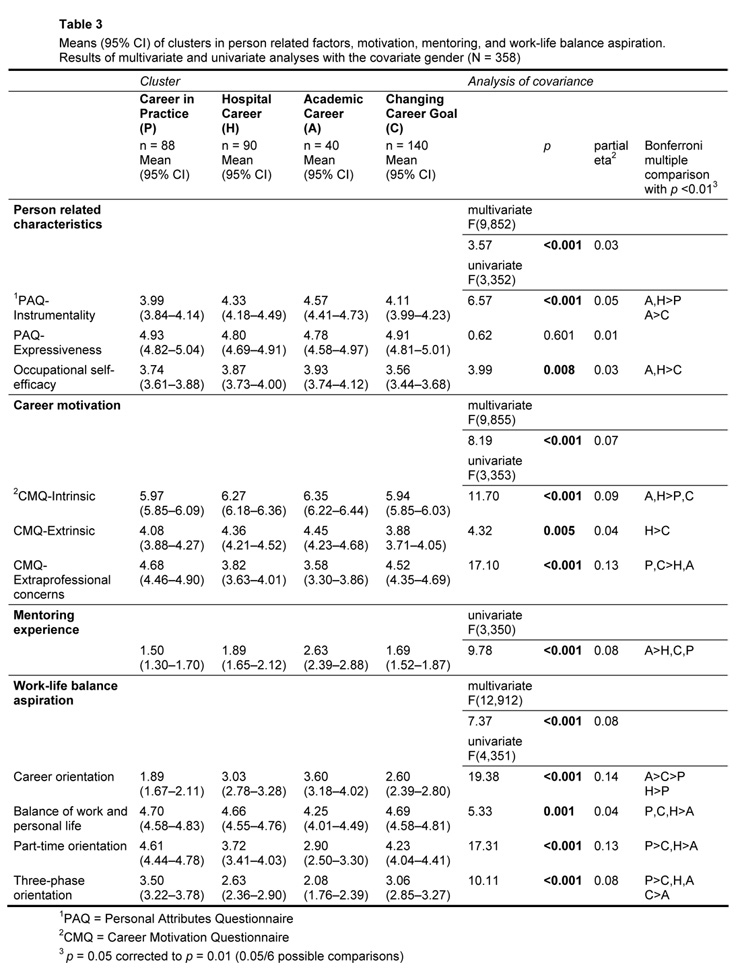
Table 3
In Cluster 1,there were 88 physicians, 24.6% of the total study sample. As seen in table 1, about 90% prioritised a career in a medical practice in various specialties (68% at T2, 100% at T3, 97% at T4, and 90% at T5). Therefore, this cluster was named Career in Practice. Ninety (25.1%) respondents were assigned to Cluster 2.About 80% of them aspired to have a career in hospital medicine (71% at T2, 100% at T3, 99% at T4, and 83% at T5). This cluster was named Hospital Career. In Cluster 3, there were 40 (11.2%) participants. Two thirds of them preferred a career in academic medicine (45% at T2, 73% at T3 and T4, and 63% at T5). This cluster was named Academic Career. In Cluster 4, 140 (39.1%) subjects were found. They showed a changing career preference from one measurement point to the other. However, none of them considered a career in academia at any assessment. This cluster was named Changing Career Goal.
Furthermore, it has to be mentioned that at T2 (i.e. in their first year of residency), 20–30% of the participants assigned to Clusters 1–3 had not yet decided on their future professional career path. While doctors in Cluster 1 and 2 rarely considered career paths other than private practice and hospital medicine respectively, some physicians in Cluster 3 (academic career) also thought about a career in hospital medicine. The respondents in Cluster 3 hardly ever considered a career in private practice or in other medicine-related fields. Cluster 4 was characterised by a high fluctuation in their career plans.
Further analyses revealed in which personal characteristics the physicians in the four clusters differed between each other (table 2). In terms of gender, female physicians were overrepresented in Cluster 1 and Cluster 4, whereas there were more male physicians in Cluster 3. In Cluster 2 the gender distribution was almost equal. The age differences between the clusters were not significant. With regard to children at T5, there was no significant correlation between cluster affiliation and having children in males, but females with children were overrepresented in cluster 1 and 4. Concerning medical specialty, physicians specialising in primary care were mainly found in Cluster 1, those in surgical fields in Cluster 2 and 3, anaesthesiologists in Cluster 2, internal medicine specialists and doctors in other medical specialties in Cluster 4.
In Table 3, the means and confidence intervals of clusters for personal characteristics, career motivation, mentoring, and work-life balance aspirations as well as the results of multivariate and univariate analyses and Bonferroni multiple comparisons are listed, all controlled for the covariate gender. Subjects in Cluster 3 (academic career) showed the highest values in instrumentality, followed by those in Cluster 2, 4 and 1. Doctors assigned to Cluster 3 also scored highest regarding occupational self-efficacy, intrinsic career motivation and mentoring. Physicians belonging to Cluster 1 (career in practice) scored high in extraprofessional concerns, but low in instrumentality and mentoring. Respondents of Cluster 4 (changing career goal) showed low values in intrinsic and extrinsic career orientation. In terms of work-life balance aspirations, physicians tracking a career in hospital medicine or an academic career did not consider to work part-time, while doctors aspiring to work in private practice did. Summarising the described cluster differences, it can be stated that physicians in Cluster 2 and 3 significantly differ from those in Cluster 1 and 4.
In table 4 the means and confidence intervals of clusters in workload, career success and career satisfaction, as well as the results of multivariate and univariate analyses and Bonferroni multiple comparisons are listed, all controlled for the covariate gender. Subjects in Cluster 2 showed a significantly higher workload than those in Cluster 1. In terms of career success, participants following an academic career rated their objective and subjective career success significantly higher than those aspiring to other career paths, especially a career in practice. However, the four clusters did not reveal a significant difference with regards to satisfaction with career.
The present paper reports follow-up data of a cohort of graduates of the three medical schools in German-speaking Switzerland [8–9]. Their postgraduate training, however, is completed at hospitals all over the country. Therefore the results reflect not only cultural and training circumstances in German-speaking Switzerland, but can be generalised for all parts of Switzerland. It has to be assumed that the variance of career and employment conditions between the language areas is not greater than within the language areas. The data provided by the 358 physicians participating at assessments over an eight-year period give important references on the career path aspirations of the younger physician generation, but are not representative for all medical school graduates in 2001.
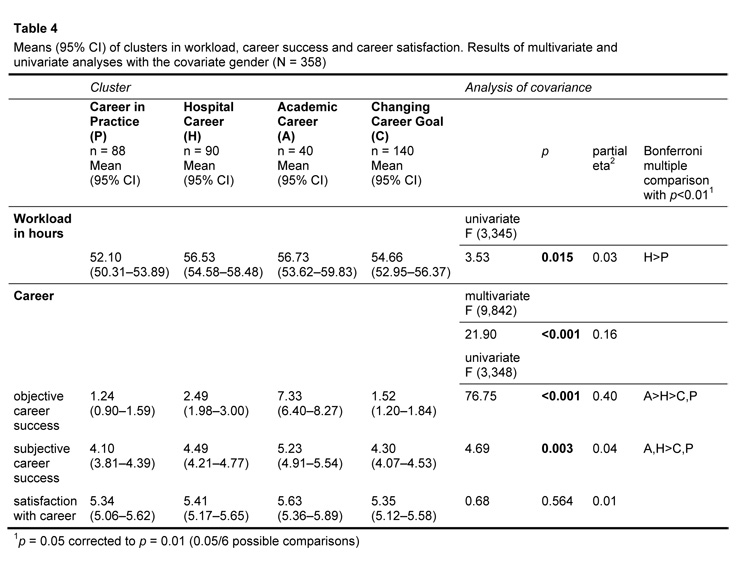
Table 4
Cluster analysis is an algorithm for sorting data [18], and provides clusters of career paths in a physician cohort that has hardly been described in the career literature [19–20]. The frequency distribution of the clusters in the current study was surprising: almost 40% of the cohort doctors switch between different career path options during their postgraduate training. It was expected that half of the study participants would choose either a career in private practice or in hospital medicine [20]. As also known from other studies [21–23], only a minority pursue an academic career. A hospital career path is more predictable and easier to schedule. Conditions for a career in academia are more competitive and there are less available posts. An academic career is more difficult to steer and does not only depend on a physician’s scientific oeuvre. Therefore, future academics often consider a hospital career rather than an academic career path.
It is striking that the career path preference in Cluster 1, 2 and 3 was so distinct. This means that the majority of physicians have made their career choice by half way through their residency at the latest. Physicians in these clusters seem to plan their career path actively. Trainees in Cluster 4, however, are less goal-oriented and seem to pursue their career path more reactively according to available job opportunities. Our data do not indicate whether subjects with changing career goals do not seek career counselling or whether they change their career goal because of inconvenient workplace conditions and inconsistencies between their personal and professional life perspectives.
As mentioned some specialties come along with certain career paths: family and general internal medicine are usually practiced in private practice; therefore subjects qualifying in these specialties are predominantly met in Cluster 1. Physicians working in surgery or anaesthesiology understandably stay in hospital pursuing either a clinical or an academic career. Cohort doctors specialising in the field of internal medicine can choose either of the three career paths.
In terms of gender, it is remarkable that female physicians, especially those with children, are overrepresented in Cluster 1 and 4. A career in private practice (Cluster 1) provides the possibility of flexitime or part-time employment, which are working conditions favoured by doctors who estimate extraprofessional concerns as equally important as their professional career [8, 24–27]. In the cluster with changing career goals (Cluster 4), there were also more females with children. When starting their residency, some female doctors still have ambitious career goals. As soon as they have children, they realise the difficulties to combine requirements of family and professional life, especially in hospital medicine, and switch between different career path options depending on their personal life situation [28–30]. Other women anticipate career obstacles in connection with parenthood from the time when they start postgraduate training, and therefore they abstain from a prestigious career, and plan their career less goal-oriented [31–32].
In Cluster 2 and 3, we found physicians showing high instrumentality, occupational self-efficacy, intrinsic and extrinsic career motivation; their attitude towards work-life balance was mainly career-oriented. As also reported by other authors, trainees who pursue a prestigious hospital or academic career need to be decisive, proactive, goal-oriented and self-confident [14, 33–34]. Subjects who do not show these characteristics to a high extent are more in doubt about their chosen career path, and they were more often found in Cluster 4. When extraprofessional concerns and part-time preference play an important role for choosing a career path, the option of a private practice is an obvious alternative [8]. A rather unfavourable alternative is to put off the definite career decision [25, 35]. As reported by other authors and with the current findings [9, 33, 36–38], mentoring reveals to have a special significance for staying on the academic career path.
Respondents assigned to Cluster 2 and 3, reported higher workload. However, the difference to those of the other clusters was not substantial although it reached the level of significance. This is due to the Swiss federal contract on working hours for residents and senior physicians, in place since 2005, limiting the workload to 50 h/week. Furthermore, most of the study participants had not yet advanced to the higher hospital or academic hierarchy, posts in which the weekly workload usually exceeds the official working hours.
Subjects in Cluster 3 showed the highest values in objective career success. This was expected because the Career Success Scale mainly addresses scientific issues and measures scientific progress [15]. Also the subjectively assessed career success was highest in this cluster. When answering this question, the respondents compare their career success with that of other doctors at the same level of postgraduate training. In the medical community, career success is mainly associated with scientific and academic career steps.
As gender was controlled in all analyses as covariate, the mentioned effects cannot be ascribed to gender differences.
A last important result is the finding that there were no differences between the clusters in terms of satisfaction with career. Other authors have reported varying satisfaction scores in physicians depending on specialty, practice, employment in a hospital or in a medical school [39], but these studies did not take the chosen career path into account. Subjects in our study, irrespective of their career path aspiration, seemed to be satisfied with their career choice as well as their career path.
Strengths and limitations of the present study have to be mentioned. The reported results are based on an eight-year follow up of a 2001 cohort of medical school graduates with a good response rate. Distinct career clusters over time could be identified. However, the follow-up sample cannot be considered as being representative for the total 2001 Swiss medical school graduate cohort.
The eight-year follow-up of the 2001 Swiss medical school graduates revealed four distinct career paths which are already seen in the trainees’ third to fourth year of residency. Medical schools and authorities for physicians’ further education as well as health politicians should set up career path counselling early in postgraduate training based on the physician’s personal characteristics and the needs of the health care system; the trainee should be supported to stay on the career path that best suits his/her personal and professional profile. Special attention should be paid to the rather large subgroup of physicians who do not decide on a certain career path or switch from one to another.
We thank Prof. Claus Buddeberg for critically revising the manuscript.
1 Chervenak F, McCullough L, Cefalo R. An ethical justification and policy for making commitments during computerized residency application processes: The US matching program as a laboratory for needed reform. Adv Health Sci Educ Theory Pract. 2009;10.1007/s10459-009-9167-1.
2 Jefferies T. Selection for specialist training: what can we learn from other countries? BMJ. 2007;334:1302–4.
3 Delamothe. Centralised application services for specialist training. BMJ. 2007;334:1285–6.
4 Gjerberg E. Gender differences in doctors’ preference – and gender differences in final specialisation. Soc Sci Med. 2002;54:591–605.
5 Dorsey ER, Jarjoura D, Rutecki GW. The influence of controllable lifestyle and sex on the specialty choices of graduating U.S. medical students, 1996–2003. Acad Med. 2005;80(9):791–6.
6 British Medical Association: BMA Cohort Study of 1995 Medical Graduates. London: British Medical Association, Health Policy & Economic Research Unit; 2005.
7 Newton DA, Grayson MS, Foster Thompson L. The variable influence of lifestyle and income on medical students’ career choices: data from two U.S. medical schools, 1998–2004. Acad Med. 2005;80(9):809–14.
8 Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. The new generation of family physicians – career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138(21-22):305–12.
9 Buddeberg-Fischer B, Stamm M, Buddeberg C, Bauer G, Hämmig O, Knecht M, Klaghofer R. The impact of gender and parenthood on physicians’ careers – professional and personal situation seven years after graduation. BMC Health Serv Res. 201;10(40).
10 Alfermann D, Reigber D, Turan J. Androgynie, soziale Einstellungen und psychische Gesundheit: Zwei Untersuchungen an Frauen im Zeitvergleich. In Androgynie Vielfalt und Möglichkeiten. Eds. Bock U, Alfermann D. Stuttgart: Metzler; 1999:142–55.
11 Abele AE, Stief M, Andrä MS. Zur ökonomischen Erfassung beruflicher Selbstwirksamkeitserwartungen – Neukonstruktion einer BSW-Skala. Zeitschrift für Arbeits- und Organisationspsychologie 2000;44:145–51.
12 Abele AE: Karriereorientierungen angehender Akademikerinnen und Akademiker. Bielefeld: Kleine; 1994.
13 Blickle G, Kuhnert B, Rieck S. Laufbahnförderung durch Unterstützungsnetzwerk: Ein neuer Mentoringansatz und seine empirische Überprüfung. Zeitschrift für Personalpsychologie 2003;2(3):118–28.
14 Abele AE. Ziele, Selbstkonzept und Work-Life-Balance bei der längerfristigen Lebensgestaltung. Zeitschrift für Arbeits- und Organisationspsychologie 2005;49(4):176–86.
15 Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Career-Success Scale – a new instrument to assess young physicians’ academic career steps. BMC Health Serv Res. 2008;8(120).
16 Abele A, Stief M. Selbstregulationskompetenzen und beruflicher Erfolg. In Individuelle Steuerung beruflicher Entwicklung: Kernkompetenzen in der modernen Arbeitswelt. Ed. Wiese B. Frankfurt: Campus; 2004:61–89.
17 Bacher J, Wenzig K, Vogler M. SPSS TwoStep Cluster – A First Evaluation. In Arbeits- und Diskussionspapiere 2004-2. Erlangen-Nürnberg: Universität Erlangen-Nürnberg; 2004.
18 Bacher J. Clusteranalyse. Anwendungsorientierte Einführung. München: Oldenbourg; 2002.
19 Jones L, Fisher T. Workforce trend in general practice in the UK: results from a longitudinal study of doctors’ careers. Br J Gen Pract. 2006;56:134–6.
20 British Medical Association: The Cohort Study of 2006 Medical Graduates. Ed. British Medical Association Health Policy & Economic Research Unit. London: British Medical Association; 2009.
21 Reichenbach L, Brown H. Gender and academic medicine: impact on the health workforce. BMJ. 2004;329:792–5.
22 Bowles A, Kevorkian C, Rintala D. Gender differences regarding career issues and promotion in academic physical medicine and rehabilitation. Am J Phys Med Rehabil. 2007;86:918–25.
23 Berweger S, Keller C. Prädiktoren der akademischen Laufbahnintention. Ergebnisse einer geschlechtervergleichenden Befragung von Doktorandinnen und Doktoranden auf dem Hintergrund der sozial-kognitiven Laufbahntheorie. Zeitschrift für Pädagogische Psychologie 2005;19(3):145–58.
24 Gjerberg E. Women doctors in Norway: the challenging balance between career and family life. Soc Sci Med. 2003;57(7):1327–41.
25 Heiligers PJM, Hingstman L. Career preferences and the work-family balance in medicine: gender differences among medical specialists. Soc Sci Med. 2000;50:1235–46.
26 French F, Andrew J, Awramenko M, Coutts H, Leighton-Beck L, Mollison J, et al. Why do work patterns differ between men and women GPs? J Health Organ Manag. 2006;20(2-3):163–72.
27 Allen I. Women doctors and their careers: what now? BMJ. 2005;331:369–72.
28 Abele AE. Gender gaps in early career development of university graduates. Why are women less successful than men? Eur Bull Soc Psychol. 2000;12(3):22–37.
29 Hoff E-H, Grote S, Hohner H-U, Dettmer S. Berufsverlaufsmuster und Geschlecht in Medizin und Psychologie. Z Politische Psychologie. 2000;8:203–23.
30 Hohner H-U, Grote S, Hoff E-H. Geschlechtsspezifische Berufsverläufe. Unterschiede auf dem Weg nach oben. Dtsch Ärztebl. 2003;100(4):A 166–9.
31 Reed V, Buddeberg-Fischer B. Career obstacles for women in medicine: an overview. Med Educ. 2001;35(2):139–47.
32 Johnson C, Johnson B, Liese B. Dual-doctor marriages: career development. Fam Med. 1992;24(3):205–8.
33 Buddeberg-Fischer B, Stamm M, Buddeberg C. Academic career in medicine – requirements and conditions for successful advancement in Switzerland BMC Health Serv Res. 2009;9(70).
34 Seibert S, Crant J, Kraimer M. Proactive personality and career success. J Appl Psychol. 1999;84(3):416–27.
35 Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990–2003. Acad Med. 2005;80(9):797–802.
36 Sambunjak D, Straus SE, Marusic A. Mentoring in Academic Medicine. JAMA. 2006;296:1103–15.
37 Bussey-Jones J, Bernstein L, Higgins S, Malebranche D, Paranjape A, Genao I, et al. Repaving the road to academic success: the IMeRGE approach to peer mentoring. Acad Med. 2006;81(7):674–9.
38 Wasserstein A, Quistberg D, Shea J. Mentoring at the University of Pennsylvania: Results of a faculty survey. Society Gen Intern Med. 2007;22:210–4.
39 Leigh J, Tancredi D, Kravitz R. Physician career satisfaction within specialties. BMC Health Serv Res. 2009;9(166).
The study was supported by grants from the Swiss National Science Foundation (NF Nos. 3200-061906.00, 3200 BO-102130, 3200 BO-113836), the Swiss Federal Office of Public Health, the Swiss Medical Association (FMH) and the Society of Swiss Residents and Senior Physicians (VSAO).