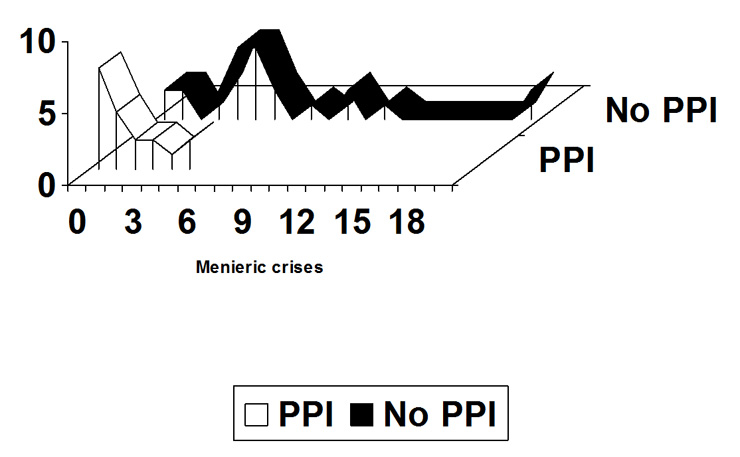
Figure 1
Frequency plot of menieric crises in the two groups of study.
DOI: https://doi.org/10.4414/smw.2010.13104
A preliminary report of a retrospective study
Meniere’s disease (MD) is a condition characterised by intensive crises of various combination of symptoms including fluctuating hearing loss, tinnitus, aural fullness and vertigo and was firstly described by Prospero Meniere more than a century ago [1]. Although many hypotheses have been postulated, its origin still remains unknown, nevertheless, MD is usually considered as the clinical expression of an endolymphatic hydrops of the inner ear. This definition has been supported by classical, pathological post-mortem examinations [2, 3] and, more recently, by MRI findings [4]. A reliable explanation for the causes of this hydrops, however, has never been identified.
In some previous papers, the possible role of proton pumps exerting their action in the inner ear during transient ischaemia was proposed to explain the pathogenesis of MD [5, 6]. This standpoint was supported by an association of several factors: the well known importance of the acid base homeostasis for the function of inner ear structures [7, 8], the possible influence of an alteration of this homeostasis in the genesis of MD [7], the reported presence of gastric-type proton pumps in the inner ear [9], and their supposed tendency to remain active during ischaemia, as observed in other organs, thus resulting in ionic concentration changes which could in turn lead to hydrops [6].
In order to seek an initial confirmation of the this hypothesis and begin to study the possibly favourable effect of the use of PPI in some inner ear affections, a preliminary investigation was performed in a sample of patients diagnosed with MD. The aim was to assess whether the assumption of PPI used for gastro-oesophageal therapeutic purposes was associated with the course of the labyrinthine disorder.
Between January 2001 and December 2006, 42 patients (24 females, 18 males) affected by MD were examined in the tertiary reference centre of the University Hospital of Bologna, Italy and in the private office of an ENT specialist (L.M.) in Cassino, Italy. The average age of these patients was 56.6 years (range 24–78 years). All patients belonged to class 2 of MD, according to the classification of the American Academy of Otolaryngology [10] (Table 1) and five patients were affected by a bilateral form of the disease. The information concerning this retrospective study was collected by means of clinical charts and a telephone call. We consecutively collected patients until we acquired sufficient number for a preliminary report. Owing to a possible lack of homogeneity of the available data, the only inclusion criterion was the careful ratification that the patients could definitively be classed as MD class 2. As this investigation was not based on updated instrumental examination, hearing function was not recorded. In fact, hearing is commonly unstable for a more or less long period in MD, especially during crises, and can deteriorate during the natural history of the affection. Therefore, in the absence of homogeneous recent data, we preferred not to mention the audiometric measurements at the time of the investigation, as these could have changed with respect to the previously recorded measurements. The interview consisted of asking patients the following three questions:
1. Have you suffered from any form of menieric crisis? (to confirm the inclusion in class 2)
2. How many crises have you had in the last 12 or 24 month period? (the immediate recall of the crisis by the patient was considered as a sufficient criterion of severity)
3. Have you used any kind of PPI? If yes; how long did you use it?
Within the study group, 18 patients (10 females and 8 males, average age 54.8 years, range 40–78 years) had been prescribed a PPI for at least 12 consecutive months for gastro-protective purposes. The type of drug, its dosage, the number of daily administrations and the date of beginning of the therapy differed from one patient to another. Ten of these patients (8 females, 2 males, average age 52 years, range 41–68 yrs.) were examined in Cassino by one of the authors (L.M).
24 patients (14 females and 10 males, average age 57.9 years, range 24–77) had never used a PPI.
We recorded the number of menieric crises reported in the observation period. The mean time between the interview and the first visit to the clinic was 21.9 months (range 9–43 months). In order to even the variable duration of the observation period of the single cases, we calculated the number of crises per year. A statistical analysis was performed by means of the x 2 test and significance was defined when p<0.05.
| Table 1: List of degrees of Meniere’s disease according to the American Academy of Otolaryngology (12). |
| 1. Certain – Definite disease with histopathological confirmation. |
| 2. Definite – Requires two or more definitive episodes of vertigo with hearing loss plus tinnitus and/or aural fullness. |
| 3. Probable – Only one definitive episode of vertigo and the other symptoms and signs. |
| 4. Possible – Definitive vertigo with no associated hearing loss. |
Within the group of patients using PPI (n=18), 13 (72.2%) presented less than one episode of menieric crisis per year, while the remaining 5 (27.8%) reported more than one episode of menieric crisis per year. On the other hand, in the group of patients who never had been prescribed a PPI (n=24), only 4 (16.7%) suffered from less than one episode of menieric crisis/year, whilst 20 (83.3%) reported more than one episode of crisis/year. Figure 1 shows the frequency plot of the crises in both groups. The difference between the two groups of study was statistically significant (p<0, 001).
The hypothesis of a favourable effect of proton pump inhibitors (PPI) on the inner ear homeostasis was inspired by the casual observation of some patients in whom tinnitus improved when using these drugs for gastro-oesophageal affections [11]. The possible effect on the labyrinth was initially attributed to the control of the reflux [11], however, our personal conviction that there is a common pathogenic mechanism in different inner ear affections led us to consider the possibility of a more direct effect of PPI on the inner ear [6, 12].
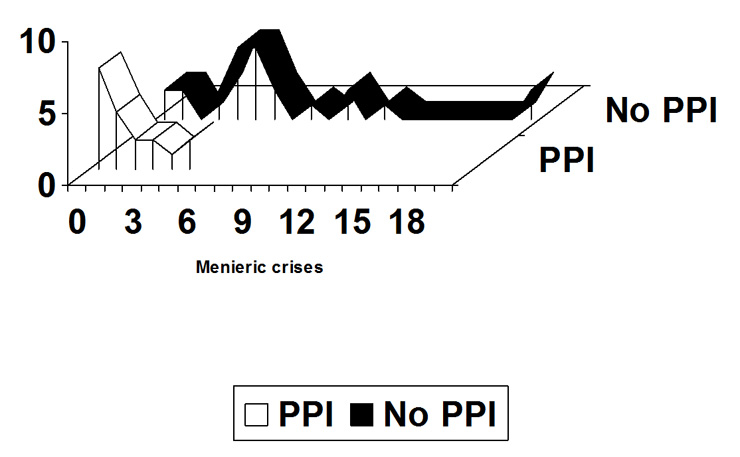
Figure 1
Frequency plot of menieric crises in the two groups of study.
The lack of instrumental investigations at the moment of the study permitted a rough match of the condition of diagnosed MD with the history of use of PPI, according to the above cited pathogenic model that, to our knowledge, was first proposed by our group [6]. In this preliminary phase, in our opinion, more specific details concerning the advancement of the affliction can be omitted. In fact, the study was fundamentally oriented to search for a relationship between two factors previously never matched. Consequently, it appeared a reasonable choice not to divide the study population into subgroups in this phase, even taking into account the fact that MD typically presents with crises at indeterminate times.
This approach was supported by the finding of a highly statistical significant difference in the number of crises reported over time by the patients of the two matched groups. In fact, users of PPI proved much less affected by menieric crises than non-users. In our opinion, this finding in itself deserves reporting, as the favourable conditions linked to PPI consumption appear too marked to be easily labelled as coincidental. Moreover, it must be outlined that this therapy, in the patients investigated, was planned and followed for reasons with no connection with MD, and with no common dosage or purpose. In fact, the activity of these drugs is reported to vary in time and in relationship with the activity of the pumps, therefore not ensuring a complete protection during the day with any of dose or route of administration [13]. This could explain the tendency to control the inner ear disturbance without achieving a total remission as was observed in the sample studied.
A limit of this study is its retrospective character, which can to some extent interfere with the availability and the precise evaluation of the data. However, due to the length of time required for a prospective investigation, and the difficulties of collecting reliable information on a representative series linked to the particular natural history of MD, a preliminary retrospective observation seemed useful. The aim was to offer some initial matter for reflection and to gather initial verification of our theoretical model [6] and to better define the topic. A longitudinal study remains mandatory.
The use of two different settings for the data collection could cause some degree of disparity in the results. On the other hand, this might also result in a more objective and free from prejudice evaluation.
In conclusion, even if the reported data at the moment only indicate that the proposed model [6] could imply interesting developments, nevertheless they strongly suggest the need for further investigation in order to better define MD and related therapeutic possibilities. As stated above, further more detailed studies are needed in order to investigate the therapeutic potentials in otologic disease. However, the observed findings, provided they can be confirmed, may represent a promising first step in this direction.
1 Ménière P. Maladies de l’oreille interne offrant des symptomes de la congestion cerebral apoplectiforme. Gaz Med de Paris. 1861;16:88.
2 Hallpike CS, Cairns H. Observations on the pathology of Ménière’s syndrome. J Laryngol Otol. 1938;53:625–55.
3 Yamawaka K. Uber die pathologisch Veranderung bei einem Ménière-Kranken. J Otorhinolaryngol Soc Jpn. 1938;4:2310–2.
4 Nakashima T, Naganawa S, Sugiura M, et al. Visualization of endolymphatic hydrops in patients with Ménière’s disease. Laryngoscope. 2007;117:415–20.
5 Pirodda A, Brandolini C, Raimondi MC, Modugno GC, Borghi C. Gastric type proton pump of the inner ear: Its possible involvement in labyrinthine disorders. Audiol Med. 2008;6:249–50.
6 Pirodda A, Brandolini C, Raimondi MC, Ferri GG, Modugno GC, Borghi C. Meniere’s Disease: update of etiopathogenetic theories and proposal of a possible model of explanation. Acta Clin Belg. 2010;65:170-5.
7 Couloigner V, Loiseau A, Sterkers O, Amiel C, Ferrary E. Effect of locally applied drugs on the endolymphatic sac potential. Laryngoscope. 1998;108:592–8.
8 Dou H, Finberg K, Cardell EL, Lifton R, Choo D. Mice lacking the b1 subunit of H+ – ATPase have normal hearing. Hear Res. 2003;180:76–84.
9 Lecain E, Robert JC, Thomas A, Tran Ba Huy P. Gastric proton pump is expressed in the inner ear and choroids plexus of the rat. Hear Res. 2000;149:147–54.
10 American Academy of Otolaryngology. Guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. Otolaryngol Head Neck Surg. 1995;113(3):181–5.
11 Pirodda A, Brandolini C, Raimondi MC, Modugno GC. The possible influence of proton pump inhibitors of the homeostasis of the inner ear. Med Hypotheses. 2009;72:325–6.
12 Pirodda A, Borghi C, Ferri GG. A different modulation of vascular endothelial growth factor (VEGF) activation in response to hypoxia could cause different clinical pictures in the inner ear disorders. Audiol Med. 2010, 8(1):33–5.
13 Metz DC, Vakily M, Dixit T, Mulford D. Review article: dual delayed release formulation of dexlansoprazole MR, a novel approach to overcome the limitations of conventional single release proton pump inhibitor therapy. Aliment Pharmacol Ther. 2009;29:928–37.