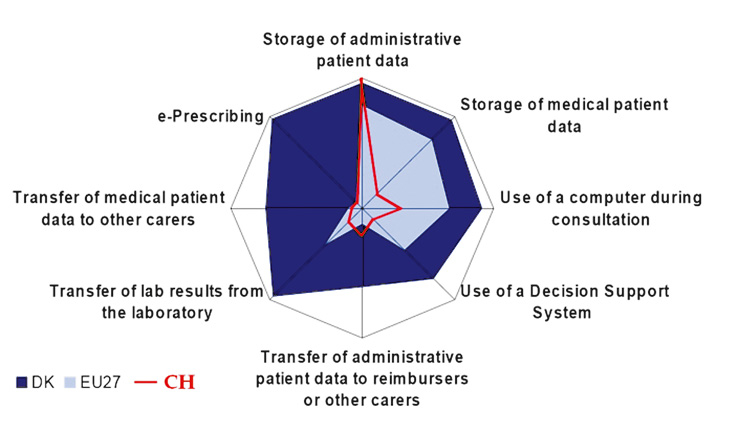
Figure 1
Use of certain IT features in Switzerland compared to the European Union modified according to [4].
DOI: https://doi.org/10.4414/smw.2010.13088
The implementation of electronic health information technologies (HIT) is seen world wide as a major target to align existing structures of care with newly arising challenges largely as a result of demographic changes. In particular, the increase of chronic diseases and multimorbidity require a proactive as well as a structured follow-up and therefore clinical information systems are a core element of the Chronic Care Model [1–2]. However, not only in chronic diseases, but also in regard to acute health problems, huge expectations are associated with electronic databases, especially electronic medical records. E-health information technologies also represent a promising approach to improve communication not only between primary care physicians, specialists, hospitals but also with patients [3]. As a consequence, HIT are regarded as a method of increasing the efficiency of the health care system in many ways.
The European Commission assessed the prevalence and use of e health information technologies in 2008 with the international Empirica Study “Benchmarking ICT use among General Practitioners in Europe” [4]. The study examined all 27 EU countries and found a huge variability in the adoption of eHealth relevant structures and processes. Switzerland was not integrated in the Empirica study since it is not a member of the European Union. In Switzerland, primary care is not only provided by GPs, but also at least partially by general internal medicine physicians, surgeons and psychiatrists. Reliable data if and to what extent these primary care physicians (PCP) use ICT in their practices were lacking. Consequently, the aim of our study was to provide data to answer this question and to reveal possible expectations but also barriers associated with the use of ICT, especially an electronic medical record (EMR).
To address a representative sample, we used the registry of the Swiss Medical Association (FMH) providing data on physicians working in independent practices. Assuming a response rate of around 60% we randomly selected 1200 physicians from the FMH data base. Together with a cover letter they recieved a self administered questionnaire and were asked to return it by fax. After four weeks the non-responders received a written reminder. Data collection started in December 2007 and was completed in February 2008.
To address specific Swiss issues, we interviewed physicians, information officers for practice information systems (PIS) and representatives of leading software companies. In addition we performed a web-based pilot study among Swiss GPs respondents, reviewed the literature of previous surveys about the implementation of PIS and involved a group of experts in eHealth technology.
The results were implemented in the questionnaire which was mainly based on tools used in surveys in the US [5] and UK [6]. The final version contained sections on the structure of the practice, IT-Infrastructure, IT-based processes and physician expectations as well as barriers concerning the professional use of IT. It was crucial to choose an adequate concept of the electronic medical record (EMR). In the literature EMR mostly refers to systems of computerised legal clinical records, used in a hospital or a physician’s office and covering the basic functionalities of computerised orders for prescriptions, computerised orders for tests, reporting for test results and physicians notes. Electronic Health records on the other hand “represent the ability to easily share medical information among stakeholders and to allow it to follow the patient through various modalities of care from different care delivering organisations” [4]. Knowing that most of the systems currently in use in Swiss offices offer only a low level of interoperability we decided to use the term “electronic medical record” (EMR) in a consensus process with our expert panel. With the four basic functions and an organised file for incoming and outgoing documents the EMR must be able to consequentially completely replace a patient paper based documentation.
We defined as key variables age, sex, language region, professional specialty, structure of practice and use of an EMR. In a pilot-application with twenty physicians we tested comprehensibility.
Data analysis: We performed a descriptive data analysis and chi-square tests for group comparisons where applicable.
719 questionnaires were received back, representing a response rate of 59.9%. Twelve questionnaires were excluded from the analysis due to missing data, so 707 questionnaires were finally analysed. Table 1 provides an overview of the participating physicians. Regarding age, gender, professional specialty and regional distribution no significant differences in the addressed sample of 1200 physicians could be revealed. Among the respondent physicians, the specialties were as follows: 360 primary care physicians (50.9%) 202 internal medicine (28.6%), 59 surgeons (8.3%), and 86 (12.1%) psychiatrists. 75.2% of the responding physicians were male and 36.9% were 55 years or older. Most physicians worked in single handed practices (57%), only 4.2% worked in a practice with more then 3 colleagues.
| Table 1Baseline data of the study sample. | |||||||
| Total* | Responders* | Non responders* | |||||
| n | % | n | % | n | % | ||
| total | 1200 | 100 | 707 | 58.9 | 493 | 41.1 | |
| specialty | primary care | 531 | 44.3 | 360 | 50.9 | 171 | 34.7 |
| psychiatry | 165 | 13.8 | 86 | 12.2 | 79 | 16.0 | |
| surgery | 136 | 11.3 | 59 | 8.3 | 77 | 15.6 | |
| specialised internal medicine | 335 | 27.9 | 202 | 28.6 | 133 | 27.0 | |
| not specified | 33 | 2.8 | 2 | 0.2 | 31 | 6.3 | |
| sex | female | 317 | 26.4 | 175 | 24.8 | 142 | 28.8 |
| male | 883 | 73.6 | 532 | 75.2 | 351 | 71.2 | |
| Age | <= 55 yrs | 779 | 64.9 | 446 | 63.1 | 333 | 67.5 |
| <55 yrs | 421 | 35.1 | 261 | 36.9 | 160 | 32.5 | |
| language | German | 819 | 63.3 | 486 | 68.7 | 333 | 67.5 |
| French | 381 | 31.7 | 221 | 31.3 | 160 | 32.5 | |
| practice | single handed | – | – | 403 | 57 | – | – |
| 2–3 colleagues | – | – | 252 | 35.6 | – | – | |
| >3 colleagues | – | – | 30 | 4.2 | – | – | |
| use of EMR | yes, complete | – | – | 83 | 11.7 | – | – |
| yes, partially | – | – | 79 | 11.2 | – | – | |
| considering* | – | – | 72 | 10.2 | – | – | |
| no* | – | – | 473 | 66.9 | – | – | |
* Group comparisons revealed no significant differences (all p >0.05); therefore p values are not displayed
A personal computer (PC) is available in nearly all practices, but only 28.1% have a PC in every consultation room, while 43.7% use a PC only at the reception desk: For primary care physicians this figure is 46.9%. A network system is installed in 44.8% of the practices, in 47.9% all or most of the work stations have internet access, while still 8.9% have no access at all. Regarding the security of the IT infrastructure, 74.7% declared that they used an antiviral software, 47.5% a software firewall against attacks to the IT system and 25.7% a hardware firewall. Encrypted communication is installed in 69.8% of the practices, in most cases that of the Health Info Net (HIN), a system provided by the Swiss society of physicians (FMH).
| Table 2IT – Infrastructure in Swiss physicians practices. | ||||||||
| PC in each cons. room | PC only at reception | Local Area Network | Inter-net (at each PC) | Anti-viral software | Software Firewall | Hard ware Firewall | Encryption | |
| Total | 28.1 | 43.7 | 44.8 | 47.9 | 74.7 | 47.5 | 25.7 | 69.8 |
| Primary care | 28.3 | 46.9 | 46.7 | 50.0 | 80.3 | 46.9 | 26.7 | 75.6 |
| Psychiatrists | 24.4 | 32.6 | 11.6 | 26.7 | 61.6 | 48.8 | 15.1 | 60.5 |
| Surgeons | 20.3 | 49.2 | 47.5 | 49.2 | 64.4 | 44.1 | 33.9 | 54.3 |
| Internists | 31.7 | 41.1 | 55.0 | 53.0 | 73.3 | 49.0 | 26.2 | 68.3 |
| Female | 26.9 | 48.6 | 32.6 | 41.1 | 69.1 | 41.7 | 18.9 | 61.4 |
| Male | 28.6 | 42.1 | 48.9 | 50.2 | 76.5 | 49.9 | 28.0 | 72.6 |
| <=55 yrs | 35.2 | 36.3 | 50.4 | 54.9 | 76.0 | 49.1 | 30.5 | 73.5 |
| >55 yrs | 16.1 | 56.3 | 35.2 | 36.0 | 72.4 | 44.8 | 17.6 | 63.5 |
| German | 32.1 | 39.9 | 50.2 | 50.0 | 78.2 | 47.7 | 29.8 | 76.5 |
| French | 19.5 | 52.0 | 33.0 | 43.4 | 67.0 | 47.1 | 16.7 | 55.2 |
| Single hand | 21.6 | 50.6 | 37.7 | 36.5 | 73.9 | 46.7 | 21.6 | 68.2 |
| 2–3 colleagues | 33.7 | 37.7 | 51.6 | 59.9 | 79.0 | 50.8 | 29.8 | 73.8 |
| >3 colleagues | 51.0 | 19.6 | 66.7 | 78.4 | 58.8 | 37.3 | 39.2 | 64.7 |
| Full EMR | 79.5 | 3.6 | 88.0 | 71.1 | 71.1 | 47.0 | 51.8 | 84.4 |
| No EMR | 13.5 | 58.4 | 31.3 | 36.6 | 73.4 | 45.9 | 19.0 | 63.4 |
Data in table represent percentages
The respondents of the survey used more than 78 different types of patient information systems (PIS), most of them dedicated to administrative purposes only. Four companies, each with more than 50 users among the respondents, share 56.6% of the market and serve exactly 400 of the 707 respondents, 134 physicians work with the PIS of eight smaller companies (10–49 respondents) and 123 are with one of the remaining 66 companies that were mentioned by 1–9 respondents each. No use of any PIS was reported by 29 participants while 41 did not answer this question at all.
Regarding the specific use of their IT, 41.3% reported searching the internet daily for medical information and 80.0% communicate via e-mail. Only 11.7% of physicians have replaced their paper based records by EMRs, another 11.2% use certain modules for instance electronic prescriptions and another 10.2% were considering the adoption of an EMR.
Table 3 displays the use of specific features of the PIS. Overall, only 11.2% of all physicians use an EMR and, as can be seen, primary care physicians have the lowest EMR user rate amongst all observed physicians, even lower than psychiatrists with 10.5%. Significantly more younger physicians (age below 55; p <0.00; chi-square test), German speaking (p = 0.01) and physicians working in group practices stated using an EMR (p <0.00). In total, 66.9% of all physicians and nearly 70% of all primary care physicians declared they were not intending to implement an EMR within the next 3 years.
| Table 3IT use in practices. | ||||||||||
| Overalle-mail use | e-mails daily | Daily medical information | Electronic speech recognition | Electronic signature | Card reader | Full EMR | EMR partially | Considering | No EMR within 3 years | |
| Total | 80.0 | 66.2 | 41.3 | 5.1 | 5.8 | 14.2 | 11.7 | 11.2 | 10.2 | 66.9 |
| Primary care | 82.0 | 65.6 | 42.2 | 4.2 | 4.4 | 14.5 | 8.9 | 10.0 | 11.9 | 69.2 |
| Psychiatrists | 65.1 | 65.1 | 32.6 | 5.9 | 5.8 | 2.3 | 10.5 | 12.8 | 8.1 | 68.6 |
| Surgeons | 81.3 | 74.6 | 40.7 | 3.4 | 5.1 | 16.9 | 16.9 | 10.2 | 6.8 | 66.1 |
| Internists | 84.7 | 65.3 | 43.6 | 6.9 | 8.4 | 17.9 | 15.8 | 12.9 | 8.9 | 62.4 |
| Female | 76.0 | 57.7 | 28.6 | 3.4 | 3.4 | 10.8 | 8.6 | 12.0 | 9.1 | 70.3 |
| Male | 81.4 | 69.0 | 45.5 | 5.6 | 6.6 | 15.2 | 12.8 | 10.9 | 10.5 | 65.8 |
| <=55 yrs | 82.4 | 70.6 | 44.8 | 5.8 | 6.9 | 13.9 | 16.1 | 14.6 | 10.5 | 58.7 |
| > 55 yrs | 76.2 | 58.6 | 35.2 | 3.9 | 3.8 | 14.6 | 4.2 | 5.4 | 9.6 | 80.8 |
| German speaking | 79.3 | 68.3 | 44.9 | 5.1 | 5.5 | 15.8 | 13.8 | 10.9 | 11.5 | 63.8 |
| French speaking | 81.5 | 61.5 | 33.5 | 5.0 | 6.4 | 10.4 | 7.2 | 11.8 | 7.2 | 73.8 |
| Single hand | 80.5 | 63.3 | 37.2 | 5.4 | 4.2 | 12.7 | 8.7 | 7.9 | 9.2 | 74.2 |
| 2-3 colleagues | 78.3 | 67.9 | 45.2 | 3.4 | 7.2 | 14.7 | 13.5 | 15.1 | 10.7 | 60.7 |
| >3 colleagues | 86.3 | 80.4 | 52.9 | 7.9 | 11.8 | 21.5 | 27.5 | 17.6 | 13.7 | 41.2 |
Data in table represent percentages
66.9% (German speaking 63.8%, French speaking 73.8%) or 473 of all respondents refuse to consider the implementation of an EMR within the next three years. The two most important concerns responsible for this negative attitude pertain to the use of computers during consultations in 57.1% of the respondents, and in 53.1% the fear that the change is too time consuming. 34.7% are concerned about aspects of data security law and 31.9% think that the cost-benefit ratio is not adequate. Regarding the barriers against using the PC during the consultation, 46.9% primary care physicians feared a worsening of the patient relationship, 27.5% assumed the computer would irritate them, 19.5% thought it might irritate the patient. This barrier is not age dependent. Dependency of their software company was indicated by only 27.7% of the participants. Barriers do not differ significantly between the two genders, only the cost-benefit ratio is mentioned more often as a barrier by female physicians (42.5%) then by male physicians (30.9%). Physicians over 55 years of age also mentioned significantly more barriers then younger ones, namely the cost-benefit ratio and the “change is not worthwhile” (p <0.00; chi-square test). French speaking physicians were also more sceptical (p <0.00 for the cost-benefit ratio (p <0.00).
| Table 4Reported barriers towards increased IT use. | |||||||||
| Cost-benefit ratio | Too time consuming | Computer in cons room | Irritates me | Irritates my patients | The relationship | Dependency of IT-Company | Change is not worth while | Security or legal concerns | |
| Total | 31.3 | 53.1 | 57.1 | 27.5 | 19.5 | 46.9 | 27.7 | 31.9 | 34.7 |
| Primary care | 37.3 | 59.8 | 61.8 | 33.7 | 22.1 | 48.2 | 31.7 | 33.7 | 36.1 |
| Psychiatry | 32.2 | 40.7 | 35.6 | 15.3 | 11.9 | 30.5 | 20.3 | 23.7 | 33.9 |
| Surgeons | 20.5 | 41.0 | 51.3 | 17.9 | 20.5 | 46.2 | 23.1 | 46.2 | 25.6 |
| Internists | 22.2 | 49.2 | 59.5 | 23.8 | 17.5 | 52.4 | 24.6 | 27.8 | 34.9 |
| Female | 42.5 | 48.8 | 54.5 | 26.0 | 21.1 | 47.2 | 27.6 | 28.5 | 35.8 |
| Male | 30.9 | 54.6 | 58.0 | 28.0 | 18.9 | 46.9 | 27.7 | 33.1 | 34.3 |
| German | 37.1 | 59.7 | 58.1 | 29.7 | 22.6 | 47.7 | 29.4 | 32.3 | 34.8 |
| French | 20.2 | 40.5 | 55.2 | 23.3 | 13.5 | 45.4 | 24.5 | 31.3 | 34.4 |
| Age <55 | 34.7 | 56.5 | 56.5 | 27.5 | 21.8 | 49.6 | 29.4 | 10.3 | 38.5 |
| Age >55 | 27.0 | 48.8 | 57.8 | 27.5 | 16.6 | 43.6 | 25.6 | 58.8 | 29.9 |
Our survey showed that the use of EMR in Switzerland remains at a very low level, especially among primary care physicians. Even though most practices provide PCs, they are mostly only used for electronic communication via email and administrative procedures. Only a minority uses all the options and features, modern EMRs can offer.
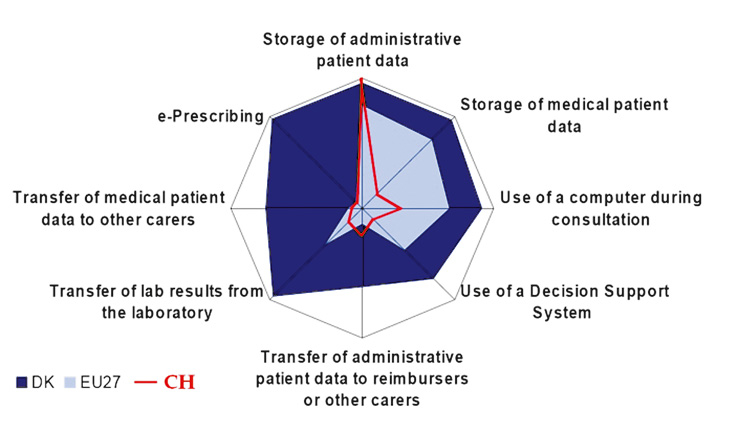
Figure 1
Use of certain IT features in Switzerland compared to the European Union modified according to [4].
Health politicians support the adoption of eHealth technology for quality reasons, but they also hope to improve control of cost in healthcare systems [7–8]. The Swiss National eHealth-Strategy as presented in 2006, aiming at implementing EMRs for the whole population in 2015 is a well articulated political aim. The discussion reached ambulatory care in Switzerland years ago, multiple publications regarding electronic patient card, health professional card, standards of interoperability and EMRs have been published recently, for example, in the “Schweizerische Aerztezeitung”, the weekly journal of the Swiss Medical Association FMH [9–12]. Despite the efforts of the national eHealth strategy and the ongoing discussion, daily practice is still far from achieving these ambitious aims. This is not only reflected in the revealed low current use of IT and EMRs in the practices but also by the alarmingly low rate of physicians willing to invest in IT within the next years. The lowest willingness to do so could be found in primary care.
As in many other countries, the role of primary care is a subject of intense discussion and several political decisions in the near past have weakened its role as, for example, the revised reimbursement for laboratory tests performed directly in the practices. One reason for the weak position of primary care is the missing data regarding the contribution of this specialty to the health care system. Electronically generated, valid data could display not only the quantitative contribution but also the qualitative contribution of primary care and could prove the need of appropriate diagnostic and therapeutic options in this setting. Evidence based quality indicators, as generated for the pay for performance programme in the UK are a convincing demonstration of quality in care [13–14]. The introduction of theses pay-for-performance programmes has not only improved quality of care but has also significantly increased GPs income [15].
In contrast to the data of the current report of the European union comparing IT use among European primary care physicians, our data revealed that only regarding “storage of administrative patient data”, Swiss physicians are at a comparable level as the mean of the 27 observed countries [4]. Regarding all other aspects, significant shortfalls are obvious, especially regarding the storage and transfer of medical patient data, e-prescribing but also regarding electronically decision support. Details of the comparison are displayed in figure 1. Denmark, which has played a leading role in implementing IT use in health care, is known to have a very efficient health care system with expenditures of about 8.8% of the BIP. Regarding the impact of IT use on the quality of care, the Commonwealth Fund International Health Policy Survey of Sicker Adults 2008 showed a clear relationship between IT use and evidence based care for chronically ill patients [16].
The results are alarming, revealing the fact that one of the richest countries in the world with one of the most expensive health care systems has obvious deficits regarding the use of IT. To enable and force IT implementation processes, the barriers and facilitators for an increased IT use have to be assessed in detail.
Not surprisingly, older physicians were less motivated to invest in IT as younger ones, in addition single handed practices were less well equipped and less willing to invest in IT. The main barriers are concerns about a worsening of the patient- doctor relationship if EMRs are used during the consultation but also a unconvincing cost-benefit ratio. These findings reveal that many physicians are still not aware of the benefits EMRs can offer, especially in the treatment and care of chronically diseases. Electronic patient records, enabling a proactive treatment, automatically generated reminders and decision support systems have been proven to improve the care of chronically ill patients [17] . In consequence they represent substantial elements of the Chronic Care Model, developed by Wagner et al. [18–19]. The costs and/or missing incentives, displayed in a worse effort/benefit relation of investments in IT, also represent a major barrier, which has to be addressed appropriately.
Furthermore it has to be acknowledged that the current fee for service system in Switzerland, with no reimbursement for quality, does not represent an optimal environment for financial invests as there is no provision for additional return on investment for the physician [20]. The revealed barriers are in line with the results of the final OECD Report on “Efficiency improvements in the Health Sector through the Implementation of ICT 2010” [21] that found the following main barriers for implementation of IT: an insufficient alignment of incentives and fair allocation of benefits and costs, a lack of commonly defined and consistently implemented standards and concerns about privacy and confidentiality.
IT and especially EMRs are underused in daily ambulatory care in Switzerland compared to other European countries. In order to increase the use of EMRs, several approaches could be helpful. First of all, the benefits of EMRs in daily routine care have to be increased, for example, by decision support systems, tools to avoid pharmaceutical interactions and reminder systems to enable a proactive treatment of chronically ill patients. Furthermore, adequate ways to offer appropriate reimbursement for the financial investments must be considered. Additional payment for quality, reflected by electronically generated, evidence based indicators, could be one promising approach as experience with the pay-for-performance programme in the UK has shown. Patients as well as physicians would benefit from more transparency and quality.
The study was financed by the Institute of Primary care and Health Services Research at the University of Zurich.
1 Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
2 Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288(15):1909–14.
3 Stone JH. Communication between physicians and patients in the era of E-medicine. N Engl J Med. 2007;356(24):2451–4.
4 Dobrev Aea. Benchmarking ICT use among General Practitioners in Europe. empirica: EUROPEAN COMMISSION Information Society and Media Directorate General 2008:116.
5 Menachemi N, Perkins RM, van Durme DJ, Brooks RG. Examining the adoption of electronic health records and personal digital assistants by family physicians in Florida. Inform Prim Care. 2006;14(1):1–9.
6 Keddie Z, Jones R. Information communications technology in general practice: cross-sectional survey in London. Inform Prim Care. 2005;13(2):113–23.
7 Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52.
8 Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. (Millwood) 2005;24(5):1103–17.
9 Denz M. Konsequenzen der nationalen E-Health-Strategie. Schweiz Ärztezeitung. 2007;9:5.
10 Giger M. E-Health 2008 – Prozesse definieren und Daten schützen. Schweiz Ärztezeitung. 2008;6:1.
11 Bhend H. Health Professional Card der Schweizer Ärzteschaft ante portas. Schweiz Ärztezeitung. 2007;42:2.
12 Oggier W. E-Health und die Arztpraxis. Schweiz Ärztezeitung. 2008;36:2.
13 Campbell S, Reeves D, Kontopantelis E, Middleton E, Sibbald B, Roland M. Quality of primary care in England with the introduction of pay for performance. N Engl J Med. 2007;357(2):181–90.
14 Falaschetti E, Campbell NR, Mohan S, Poulter N. Implementation of pay for performance policy in England. Hypertension. 2009;54(1):e5.
15 Campbell SM, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Engl J Med. 2009;361(4):368–78.
16 Schoen C, Osborn R, How SK, Doty MM, Peugh J. In chronic condition: experiences of patients with complex health care needs, in eight countries, 2008. Health Aff. (Millwood) 2009;28(1):w1–16.
17 Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, Owens DK. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296(4):427–40.
18 Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13(4):299–305.
19 Wagner EH, Groves T. Care for chronic diseases. BMJ. 2002;325(7370):913–4.
20 Ludwick DA, Doucette J. Primary Care Physicians’ Experience with Electronic Medical Records: Barriers to Implementation in a Fee-for-Service Environment. Int J Telemed Appl. 2009;2009:853524.
21 Achieving Efficiency Improvements in the Health Sector through the Implementation of Information and Communication Technologies [http://ec.europa.eu/health/eu_world/docs/oecd_ict_en.pdf]