Emergency physician intershift handover – can a dINAMO checklist speed it up and improve quality?
DOI: https://doi.org/10.4414/smw.2010.13085
Summary
BACKGROUND: Physician intershift handover has been identified as an area of high risk for adverse events, representing a critical step in patient care transition. Due to frequent shift changes and high patient numbers, emergency departments offer an ideal study setting.
AIM OF THE STUDY: At a tertiary care hospital emergency department we aimed to reduce the time needed for patient handover while maintaining or improving quality of information passed between shifts.
METHODS: Between 31 March and 20 June 2008 we observed intershift handovers in all non-surgical patients at 8 a.m. between nightshift and dayshift. We collected data on handover characteristics and patient demographics. After the usual clinical rounds following each handover, we asked senior physicians about missing or wrong information and possible implications for patient management. From 31 March to 9 May pre-interventional observation took place. On 13 May the dINAMO checklist with five items and a standardised feedback following each handover was introduced. Post-interventional observation lasted until 20 June.
RESULTS: 61 handovers totalling 23.4 hours of observation time covered 1011 patients. The intervention using the dINAMO checklist reduced mean handover time by 26% from 99 ± 3.3 to 73 ± 2.8 seconds per individual patient (p <0.0001). This resulted in a reduction of morning handover duration from 30 to 20 minutes. Senior physicians reported insignificant improvement of quality of handover. A significant decline in missing or wrong information from 194 incidents in 496 patients to 78 in 470 patients was recorded.
CONCLUSIONS: An intervention consisting of a simple checklist of five items (dINAMO) and an immediate feedback on quality not only contributes to a significant shortening of time needed for physician intershift handover in a university hospital emergency department, but simultaneously helps to improve quality of information and therefore patient management.
Introduction
Physician intershift handover involves the transfer of both responsibility and accurate, reliable patient information, and plays an important role in safe and continuous patient care [1, 2].
It is well known that both patients and physicians are affected adversely by deficiencies in the handover process [3]. Several studies have presented extensive lists of medical and organisational information to be included in handovers [2–5]. Intershift handovers take up considerable time during which physicians are unavailable for direct patient care. This issue is very critical for emergency departments (ED) where intershift handovers are frequent and patient turnover and acuity of disease are problematic. Handover quality should therefore not only be measured in quality of information transferred between physicians but also in time required.
Patients and methods
The ED of our tertiary care university teaching hospital has an annual patient census of 41 500. Handover sessions take place three times a day. All handovers between ED physicians concerning non-surgical patients present in the ED at 8 a.m. weekdays between 31 March and 20 June 2008 were studied.
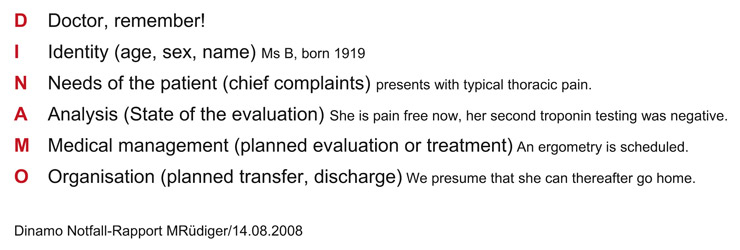
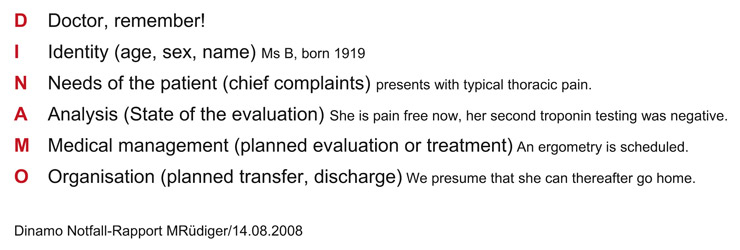
Figure 1
Six item mnemonic checklist (dINAMO) used in the intervention. Aim of the checklist was to make the reporting physician concentrate on relevant information with brevity and on the other hand give listeners an opportunity to check if all necessary items had been handed over.
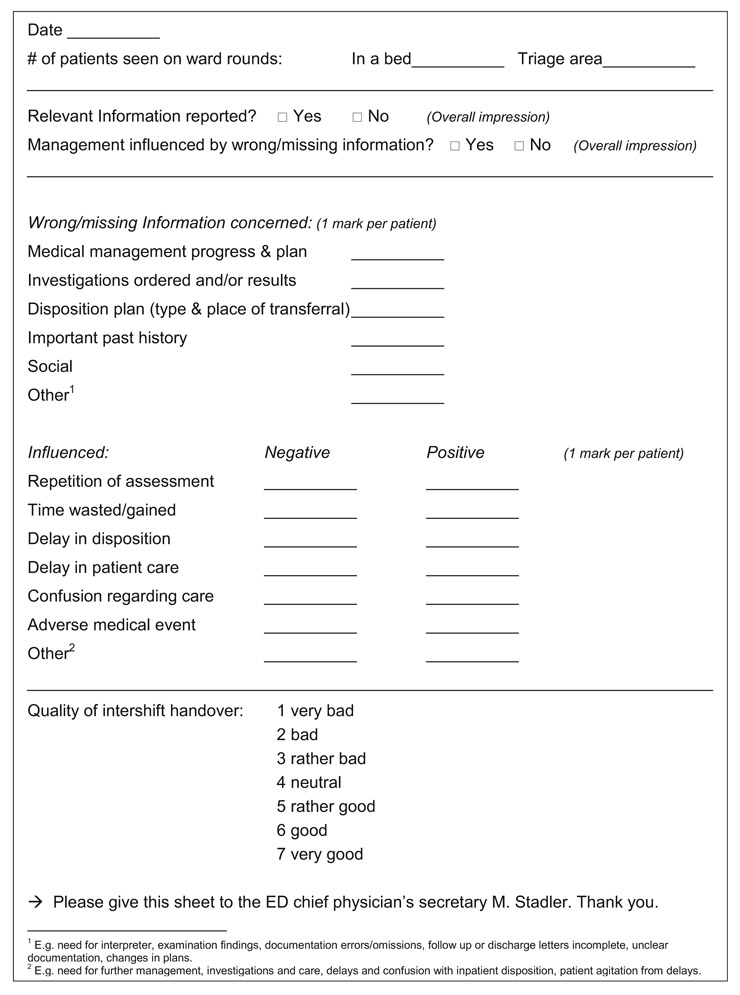
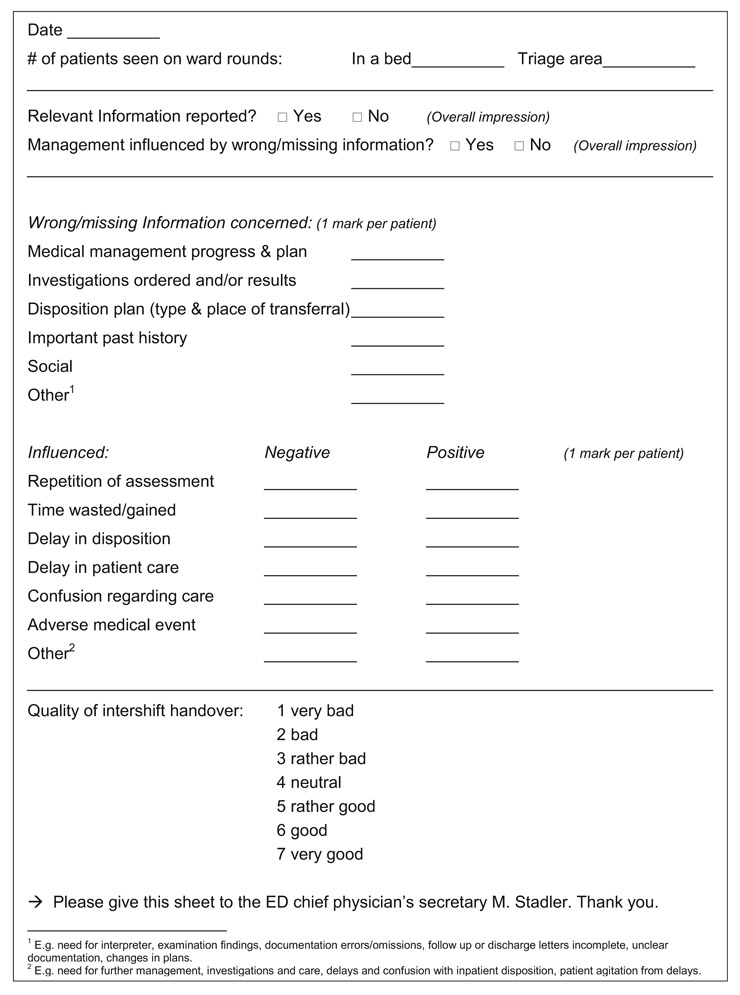
Figure 2
Post-clinical rounds questionnaire of senior ED physicians. Missing or wrong information as well as adverse events were counted. Each category could be mentioned only once per patient.
The observation of 30 pre- and 31 post-interventional handover sessions and the continuous post-handover questioning of senior ED physicians were prospectively recorded. The pre-interventional period lasted from 31 March to 9 May and the post-interventional survey took place between 13 May and 20 June. During the intervention period eleven residents and nine senior physicians were instructed to use a mnemonic checklist with five items (dINAMO) as a structural aide for handovers (fig. 1). Instruction by the chief emergency physician took approx. five minutes and included his statement on the importance of precise and short handovers as well as one example of how the mnemonic should be used. We developed the mnemonic dINAMO on the basis of published checklists with a special focus on contents and time efficiency, and tried to make it self-explanatory. The head or deputy head physician provided short feedbacks on quantitative compliance with this checklist to the reporting resident immediately after each handover session. Residents with at least one year’s work experience rotate to our ED for a minimum of six months. Rotations start every three months. Senior physicians’ education varied widely with a range from board approval to decades of experience and regular work in the ED.
Intershift handover took place in a separate room on the ED’s premises. Oral handover was based on a list of patients and supported by the use of electronic patient records visible to all participants via a high-definition TV screen. While residents reported on each patient, written information and lab results were shown to receiving physicians by a senior physician. Any missing information could be asked for or was supplemented by other participants, physicians and nurses alike. Inquiries and discussions were encouraged in pre- and post-intervention phases. Regular participants were three residents, two senior physicians, one shift-supervising nurse, and either the head or deputy head physician of the ED. Additionally, the head nurse, interns, students, and a social worker could be present.
Information on the duration of handovers, numbers of patients, interruptions (i.e. phone requests, late arrivals), participants and patient characteristics were prospectively recorded by the authors. All physicians were aware that intershift handovers were observed, both in the pre-intervention and post-intervention phase.
Senior physicians were questioned on quality of handover following completion of their clinical rounds. Items asked included the number of patients handed over whom they had personally seen, the overall quality of the handover (analogue scale of 1 to 7: 1 = very bad, 2 = bad, 3 = rather bad, 4 = neutral, 5 = rather good, 6 = good, 7 = very good), as well as the questions “Did you receive all relevant information during the handover?” and “Was patient management influenced by missing or wrong information?” (fig. 2). The senior physician was asked, in respect of each patient, whether any information had been missing or wrong, and if there were subsequently any implications for the patient’s management. Six predefined categories adapted from Ye et al. [3] (fig. 3) were used.
Statistical methods
All authors were responsible for data collection. Data was transferred into Excel spread sheet (Microsoft, Redmond, SA). Statistical analyses were performed using Gstat. For results with normal distribution mean values ± standard error of the mean (S.E.M.) were calculated and unpaired two sided t-test was used. T-test was also used for the calculation of interrater reliability. Statistics for the number of missing or wrong information items and their sequelae were performed using chi square test and Fisher’s exact test.
Results
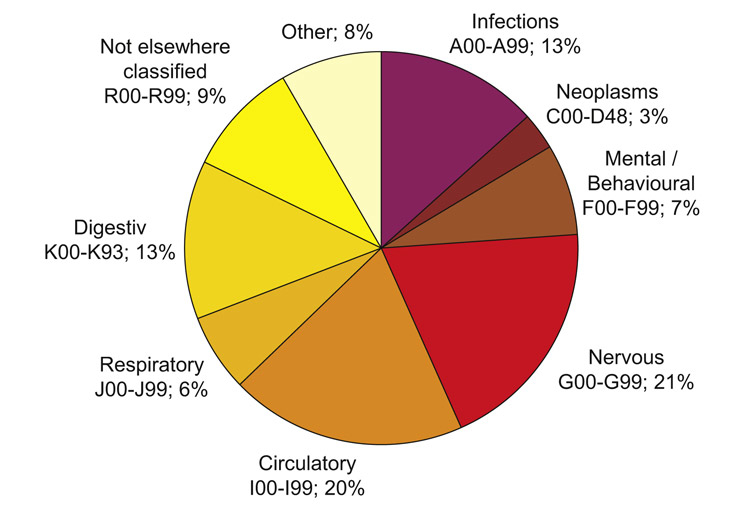
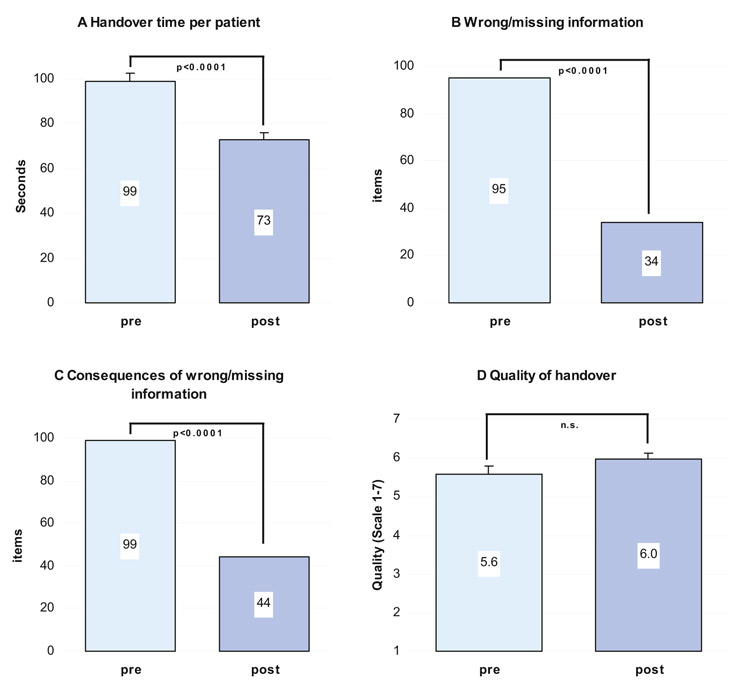
A total of 1011 patient handovers were observed during 61 sessions, 519 before and 492 after the intervention using the dINAMO checklist (38% of 2672 non-surgical ED patients). This resulted in 23.4 hours of observation (sum of duration of all handover sessions). Patients had an average age of 65 ± 20 years, 52% were men (n = 521), 48% were women (n = 490). Information on the Emergency Severity Index (ESI) was available for 652 patients (64%): 1% ESI 1, 14% ESI 2, 81% ESI 3, 3% ESI 4 and 1% ESI 5 [6]. The distribution of diagnoses at presentation is shown in fig. 3. Median number of patients per handover session remained 18.0 (range 9–27) before and after the intervention. Senior physicians completed rounds on 966 (96%) of the 1011 patients handed over. The remaining 45 patients were transferred without being seen by a senior physician (e.g. for coronary intervention, transfer to the ICU). There was a trend in improvement of the overall quality as rated by senior physicians from 5.6 ± 1.1 before to 6.0 ± 0.8 on a 7-point scale after the intervention, but this did not reach significance (fig. 4D). For physicians who rated quality for more than three pre- and postinterventional days, interrater reliability was not significantly different (p >0.1). Missing or wrong information declined significantly (p = 0.003) from a mean 3.4 items per day before the intervention to a mean 1.2 following the intervention (fig. 4B). This decline was accompanied by a shift in contents (table 1). Simultaneously, a decrease could be observed in the number of adverse events due to this missing or wrong information (fig. 4C, tables 1 and 2). No fatalities were associated with the wrong or missing information. Mean duration of handover per single patient was reduced by 26% (p <0.001) from a pre-interventional 99 ± 3.3 seconds to a post-interventional 73 ± 2.8 seconds (fig. 4A). Per session, 2.8 ± 2.1 interruptions occurred: pre-intervention 3.2 ± 2.2, and 2.4 ± 1.9 post-intervention. A mean of 8.5 persons attended handovers. Multiplying the number of participants by duration of the mean handover time, the sum of working hours was reduced by one third, from 4.2 hours to 2.8 hours.
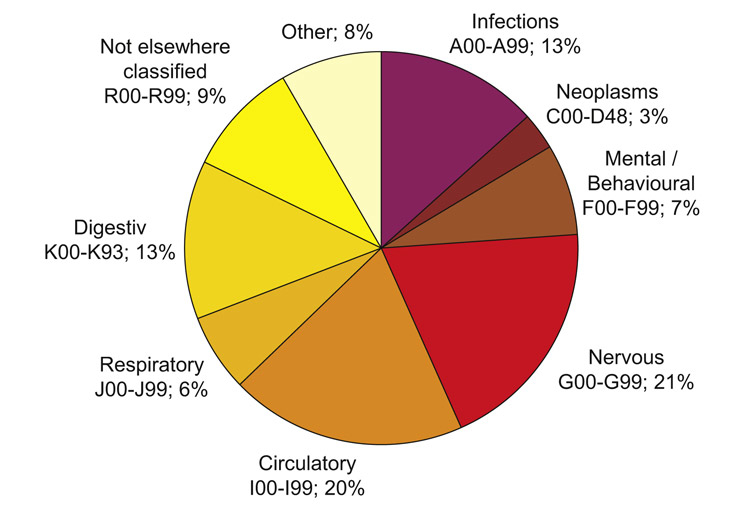
Figure 3
Distribution of ICD 10 coded diagnoses. Selection of ICD10 chapter took place during intershift handover session by the observing study physician based on information transferred during handover session. The category “not elsewhere classified” encompasses the cases where a non-specific symptom (such as weakness) remained the diagnosis whereas “other” are cases of precise diagnoses from ICD10 chapters that were seen only sporadically.
|
Table 1Missing or wrong information given in handovers as judged by senior ED physician in the post-handover survey. |
|
Missing or wrong information (n = 996)
|
|
pre
|
post
|
p |
|
Type of information
|
n
|
% |
n
|
% |
|
|
Disposition plan
|
38 |
40 |
11 |
32 |
<0.001 |
|
Medical management
|
28 |
29 |
12 |
35 |
<0.05 |
|
Investigations
|
14 |
15 |
3 |
9 |
<0.05 |
|
Past history
|
5 |
5 |
3 |
9 |
|
|
Social
|
5 |
5 |
3 |
9 |
|
|
Other
|
5 |
5 |
2 |
6 |
|
|
Sum
|
95
|
100 |
34
|
100 |
<0.0001 |
| Pre = pre-interventional handovers, post = post-interventional handovers, n = number of incidences per handover session; each category could be mentioned only once per patient. Chi square and Fisher’s exact test. |
|
Table 2Consequences of missing or wrong information given in handovers as judged by senior ED physician in the post-handover survey. |
|
Consequences of wrong or missing information (n = 996)
|
|
pre
|
post
|
p |
|
Type of consequence
|
n
|
% |
n
|
% |
|
|
Repetition of assessment
|
26 |
26 |
17 |
39 |
|
|
More time necessary
|
26 |
26 |
11 |
25 |
<0.05 |
|
Delay of disposition
|
21 |
21 |
13 |
30 |
<0.05 |
|
Delay of care
|
10 |
10 |
2 |
5 |
<0.05 |
|
Confusion
|
9 |
9 |
1 |
2 |
<0.05 |
|
Adverse medical effect
|
3 |
3 |
|
|
|
|
Other
|
4 |
4 |
|
|
|
|
Sum
|
99
|
100 |
44
|
100 |
<0.0001 |
| Pre = pre-interventional handovers, post = post-interventional handovers, n = number of incidences per handover session; each category could be mentioned only once per patient. Chi square and Fisher’s exact test. |
Discussion
Our results show that physician intershift handover in an emergency department can be speeded up by a simple intervention while simultaneously improving quality.
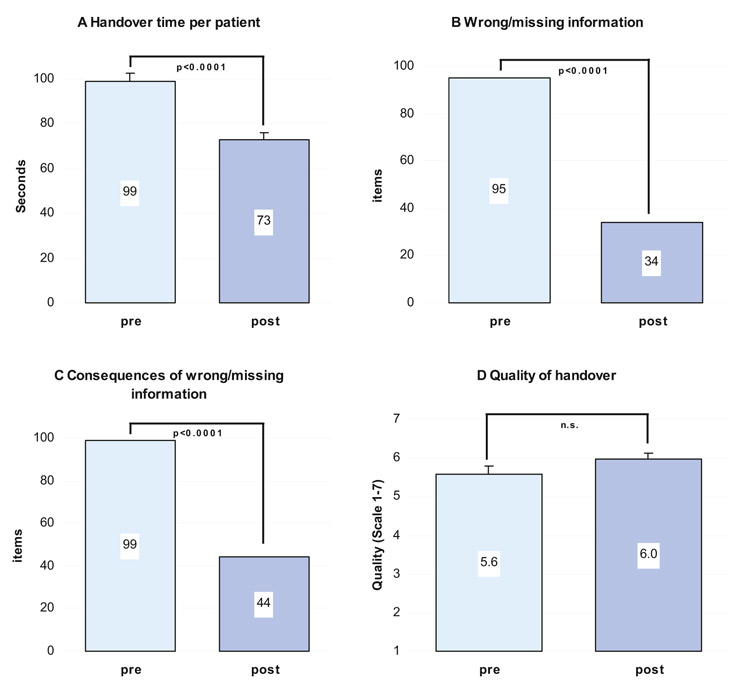
Figure 4
Handover quality before (pre) and after (post) “dINAMO”
Numbers in bars depict mean value (panel A & D) or total events (panel B & C). Bars represent S.E.M where present. Significance calculated by t-test.
Panel A: Handover time per patient. Mean time required for handover declined from 98 before the intervention to 72 seconds after the intervention.
Panel B: Wrong/missing information. Handover informational items missing or wrong judged by the senior ED physician after ward rounds.
Panel C: Consequences of wrong/missing information. Preventable adverse events secondary to missing or wrong items during the handover, judged by the senior ED physician after ward rounds.
Panel D: Quality of handover. After the ward rounds the senior ED physician rated the quality of the previous handover on a 7 point scale: 1 = very bad, 2 = bad, 3 = rather bad, 4 = neutral, 5 = rather good, 6 = good, and 7 = very good. The rating did not significantly differ between the two groups (n.s.).
The physicians observed and senior physicians rating quality and missing information did not change during the study period. Both the locations and other environmental factors remained unaltered. Although physicians were told that they were observed and received immediate feedback on their quantitative performance after handovers, they did not realise that the primary interest of the study was the time issue. Even if the time gain of around 10 minutes per handover session seems small, this can be important to both patients and physicians – especially if it is considered that handovers take place repetitively over the day and many people are involved.
Patient characteristics (such as age and complexity) influence both time needed for handover and completeness of information [7]. The majority of the patients present in the ED at 8 a.m. had an ESI of 3 (81%) and were aged over 65 (53%), which simply represents the cohort with a greater length of stay (for more detail see online Appendix 1). Most of our ED patients are discharged directly (71%). However, among non-trauma patients the admission rate was 60% and the 8 a.m. cohort typically await daytime diagnostic tests or transfer to an in-house ward or geriatric hospital.
In a study by Ye et al. in a comparable setting, a post-handover survey revealed similar results for handover time and overall quality of handover sessions compared with our pre-intervention period.
Our study has several limitations. Causes of poor perceived quality and missing or wrong information cannot be explained. We observed only one of a total of three handover sessions each day. Information could have gone missing or been reported wrongly in one of the previous handovers, or the patients’ condition could have changed unknown to the physician. The night shift did not routinely have personal contact with all patients handed over by the previous shift, but only if deemed necessary by the responsible nurse or if, for example, laboratory results rendered this necessary. Secondly, some degree of Hawthorne effect could have influenced our study results because all the participants were aware of the study. New physicians started their rotation on the ED on 1 April, and were thereby present on the ED during the whole study period. The Hawthorne effect would have similarly influenced the pre- and postinterventional phase and may therefore be minor. The post-handover questioning was based on subjective impressions and open to varying interpretation by senior ED physicians.
Quality of handover before the intervention was already rated very high, with an average of 5.6 out of 7 points. This could be due to the fact that many physicians saw no need for improvement of handovers and they were generally content. The high rating left little room for improvement. Even though wrong/missing information and its consequences declined significantly (fig. 4B and 4C), improvement in quality did not reach significance. This may be explained by the fact that subjective rating of quality took into account more criteria than those on which we questioned the physicians, e.g. the verbal style of handover and the personal relationship between reporting and qualifying physician. Knowledge of some patients from previous shifts may also influence a senior physician’s rating of quality.
Frequent changes of residents (every six months), as well as the different levels of experience between the residents (from one year to fully board approved), lays a study like this open to factors that cannot be controlled for.
Compared with the environment of handovers described or requested by other studies [8, 9], several requirements were already in place in the pre-interventional period, e.g. a fixed time of handover, a quiet room, presence of all the important participants, access to electronic patient information, combination of oral and written handover, moderation by a senior physician. Nevertheless it was possible to speed up emergency physician intershift handover and improve quality by a simple “dINAMO”.
Appendix 1
|
1A Patient gender before and after the intervention
|
| Gender (n = 1011) |
| |
Pre |
Post |
Total |
| |
n |
% |
n |
% |
n |
% |
| Male |
275 |
53 |
246 |
50 |
521 |
52 |
| Female |
244 |
47 |
246 |
50 |
490 |
48 |
|
Sum
|
519
|
100
|
492
|
100
|
1011
|
100
|
|
1B Patient age in years before and after the intervention.
|
| Age (n = 1011) |
| |
pre |
post |
| |
mean |
SD |
mean |
SD |
| Men |
64 |
18.2 |
64 |
18.1 |
| Women |
68 |
21.4 |
66 |
21.1 |
|
Sum
|
66
|
19.9
|
65
|
19.7
|
|
1C ESI Classification of patients before and after the intervention.
|
| ESI Classification (n = 1011) |
| |
pre |
post |
| |
n |
% |
n |
% |
| ESI1 |
3 |
0.6 |
2 |
0.4 |
| ESI2 |
55 |
10.6 |
38 |
7.7 |
| ESI3 |
298 |
57.4 |
227 |
46.1 |
| ESI4 |
15 |
2.9 |
7 |
1.4 |
| ESI5 |
6 |
1.2 |
1 |
0.2 |
| Missing |
142 |
27 |
217 |
44.1 |
|
Sum
|
519
|
100
|
492
|
100
|
|
1D ICD 10 coded diagnosis for patients’ major problem before and after the intervention.
|
| ICD 10 coded diagnosis (n = 1011) |
| |
pre |
post |
| ICD 10 chapter |
n |
% |
n |
% |
| Infections A00-A99 |
70 |
13 |
64 |
13 |
| Neoplasms C00-D48 |
14 |
3 |
18 |
4 |
| Mental/Behavioural F00-F99 |
42 |
8 |
33 |
7 |
| Nervous G00-G99 |
117 |
23 |
81 |
16 |
| Circulatory I00-I99 |
108 |
21 |
88 |
18 |
| Respiratory J00-J99 |
27 |
5 |
38 |
8 |
| Digestive K00-K93 |
69 |
13 |
62 |
13 |
| Not elsewhere classified R00-R99 |
43 |
8 |
53 |
11 |
| Other chapters |
29 |
6 |
55 |
11 |
|
Sum
|
519
|
100
|
492
|
100
|
Correspondence:
Prof. Dr. med. Roland Bingisser
Chefarzt Notfallstation
Universitätsspital Basel
Petersgraben 4
4031 Basel
Switzerland
rbingisser@uhbs.ch
References
1 Perry S. Transitions in care: studying safety in emergency department signovers. Nat Patient Saf Found. 2004;7:1–3.
2 Kerr M. A qualitative study of shift handover practice and function from a socio-technical perspective. J Adv Nurs. 2002;37:123–34.
3 Ye K, Taylor D, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas. 2007;19:433–41.
4 Sandlin D. Improving patient safety by implementing a standardized and consistent approach to hand-off communication. J Perianesth Nurs. 2007;4:289–92.
5 Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;11:646–55.
6 Tanabe P, Gimbel R, Yarnold PR, Adams JG. The Emergency Severity Index (version 3) 5-level triage system scores predict ED resource consumption. J Emerg Nurs. 2004;30:22–9.
7 Stiell A, Forster AJ, Stiell IG, van Walraven C. Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ. 2003;169:1023–8.
8 Singer JA, Dean J. Emergency physician intershift handovers: an analysis of our transitional care. Pediatr Emerg Care. 2006;10:751–4.
9 Safe handover: safe patients. Guidance on clinical handover for clinicians and managers. Kingston: Australian Medical Association 2006;1–45.