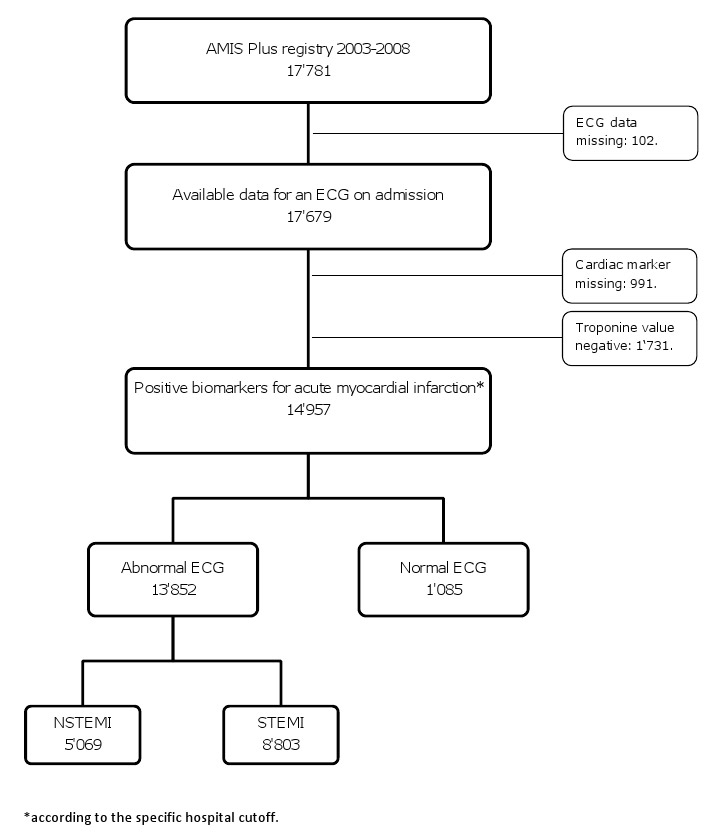
Figure 1
Overview of the patients included in this study.
DOI: https://doi.org/10.4414/smw.2010.13078
Evaluating patients with acute myocardial infarction (AMI) and administering the best available therapy remains a challenge for all practising physicians. Strategic decision-making and clinical assessments leading to a diagnosis suggesting AMI need to take place rapidly in order to justify treatment and optimise outcome. Current diagnostic guidelines rest upon clinical, electrocardiographic and biochemical evidence. The ECG has become an indispensable tool for all clinicians dealing with suspected AMI. ECG evidence is obtained rapidly, is widely available and shows reliable ischaemic signs; it therefore plays a key role in the early diagnosis of AMI and, by dividing AMI patients into ST elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) groups, provides the criteria on which the current treatment guidelines are based [1–2].
However, there are AMI patients who present with an ECG lacking all the expected changes and whose diagnosis must be established on the basis of the presenting symptoms and cardiac markers. Several previous studies suggested that AMI patients with a normal ECG can be stratified into a low-risk group and have a favourable prognosis [3–5].
The present study aims to assess AMI patients with a normal/nonspecific ECG on admission and compare them with regard to clinical features, treatment and outcome with patients whose admission ECG shows changes.
The patient data used for this study were provided by AMIS Plus, a nationwide register recording data on hospitalisation for acute coronary syndromes (ACS). Details of the AMIS Plus Project have been published elsewhere [6–10].
All patients included in this study fulfilled the criteria for enrolment in the AMIS Plus database and were admitted to participating hospitals in Switzerland between January 2003 and December 2008 with a diagnosis of AMI, which was defined as characteristic clinical symptoms and/or a typical ischaemia ECG pattern and troponins, elevated above the individual cut-off level for AMI of each particular hospital and with a valid ECG on admission. All patients are considered to have met the criteria for the ESC-ACC 2000 definitions for AMI [11]. Patients with missing data on the on admission ECG or on the cardiac marker value, and those with a discharge diagnosis of unstable angina, were excluded.
The 12-lead ECG obtained on admission was interpreted by the hospital physicians on duty at that time and the findings were captured in the AMIS Plus questionnaire. An ECG was defined as abnormal when it showed one or more of the following changes: ST-segment elevation or depression, T-wave changes, Q-waves, and left or right bundle branch blocks. Moreover, if an ECG was referred to as abnormal due to ST-segment elevation and/or a presumed new left bundle branch block, it was categorised as STEMI; if it was referred to as abnormal due to one or more of the other irregularities mentioned, it was categorised as NSTEMI. An ECG was defined as normal when it showed the usual pattern, i.e. without pathologic signs, or as non-specific when it showed minor non-ischaemic changes and did not fit the above-mentioned criteria. The patients who met the inclusion requirements were divided according to the pattern of the ECG on admission into two groups: Group 1 patients presented with normal/non-specific ECG findings and Group 2 with abnormal ECGs on admission.
Counts and percentages were used to describe discrete variables; means with standard deviation (SD) and median values with interquartile ranges (IQRs, 25th, 75th percentile) were used for continuous variables. In univariate tests, the chi-squared test and Fisher’s exact test were used for discrete variables and the unpaired t-test or the Mann-Whitney U test for continuous variables. A multivariate logistic regression model with backward stepwise variable selection was used to determine if a normal/non-specific ECG on admission adjusted for age, sex, cardiopulmonary resuscitation before admission, heart rate, systolic blood pressure, ACS with ST elevation, Killip class, history of coronary artery disease, hypertension, diabetes, dyslipidaemia, current smoking, obesity (body mass index >30 kg/m2) and primary percutaneous coronary intervention (PCI) is a predictor of in-hospital mortality. A p value lower than 0.05 was considered statistically significant. SPSS (version 15.0, SPSS Inc., Chicago, Ill) was used for all statistical analyses.
Between January 2003 and December 2008, 17 781 patients with an ACS were enrolled in the AMIS Plus registry. Cardiac marker values were missing in 991 cases and troponin values were negative in 1731 cases, which were therefore excluded. Among the 15 059 patients with elevated cardiac markers indicating AMI, another 102 cases were excluded due to missing ECG data. The remaining 14 957 patients met the inclusion criteria.
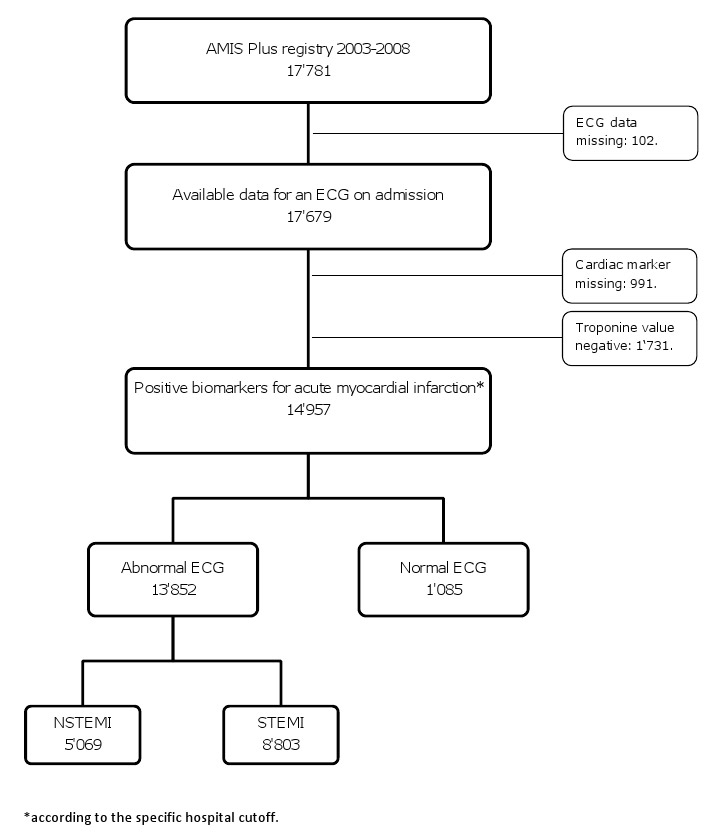
Figure 1
Overview of the patients included in this study.
1085 patients (7.3%) presented with a normal/non-specific ECG and 13 872 (92.7%) had an abnormal ECG. Among the group with an abnormal ECG, 8803 patients had STEMI (58.9%) and 5069 (33.9%) NSTEMI (fig. 1)
The baseline characteristics of AMI patients according to their admission ECG are shown in table 1.
There was no difference between the two groups in age, gender, diabetes, hypertension, family history of premature CAD or smoking habits. Dyslipidaemia, history of ischaemic heart disease and obesity (BMI >30) were significantly more frequent among the patients with a normal/non-specific ECG. However, they more frequently had lower Killip classes but similar comorbidities.
Patients with a normal/non-specific ECG presented with a longer delay (280 min; IQR 130, 835 min) after symptom onset than those with an abnormal ECG (230 min; IQR 115, 654 min), but this difference was not significant. Moreover, the patients who presented in the first 3 hours after symptom onset more often had an abnormal ECG (40.7% vs. 34.4%; p = 0.002), whereas a higher percentage of the patients presenting more than 12 hours after symptom onset (28.0% vs. 23.2%; p = 0.002) had a normal/non-specific ECG (fig. 2).
Patients with a normal/non-specific ECG at admission were given less intensive treatment; both pharmacological and interventional (table 2). They underwent significantly less frequently early PCI and the interventions took place after a longer in-hospital delay (589 min, IQR 194, 1449 min vs. 96 min; IQR 35, 341 min). However, performed coronary artery bypass grafting (CABG) was comparable between both groups.
Angiographic findings have been recorded in AMIS Plus since 2005 and are depicted in figure 3. Patients with a normal/non-specific ECG (n = 604) showed significantly higher rates of left ventricular ejection fraction (LVEF): the LVEF was above 50% in 81.3% of these patients, 15.6% had an LVEF between 35% and 50% and 3.1% had an LVEF below 35%. The rates were lower in the group of patients with an abnormal ECG (n = 7736); 55.4%, 36.6% and 8.0% respectively.
Despite the differences in therapeutic strategy the two groups had similar rates of re-infarction and cerebrovascular event, but the patients whose ECG at admission showed changes more often developed cardiogenic shock during their hospital stay and had a higher in-hospital crude mortality rate of 6.0%, compared with 3.1% in the group with a normal ECG (OR 1.91: 95%CI 1.36-2.67; P <0.001) (table 3).
In the multivariate logistic regression model a normal/non-specific ECG on admission was not an independent predictor of in-hospital mortality; adjusted OR was 0.61 with a 95% CI from 0.34–1.11 (P = 0.104). Normal/nonspecific ECG was the only non-significant variable in this model, whereas age, history of diabetes, smoking, Killip class, STEMI, history of dyslipidaemia, heart rate, systemic blood pressure, resuscitation prior to admission and PCI were significant.
| Table 1Baseline characteristics according to the patient’s ECG on admission. | |||
| Demographics | |||
| Women | 304/1085 (28.0) | 3850/4154 (27.8) | 0.86 |
| Men | 781/1085 (72.0) | 10 022/10 803 (72.2) | 0.86 |
| Age for women in years, mean ± SD | 71.9 ± 13.2 | 71.9 ± 12.6 | 0.96 |
| Age for men in years, mean ± SD | 62.9 ± 13.1 | 63.6 ± 13.1 | 0.14 |
| BMI, kg/m2, mean ± SD | 27.2 ± 4.4 | 26.8 ± 4.3 | 0.003 |
| Cardiovascular risk factors | |||
| Diabetes | 188/1049 (17.9) | 2605/13 373 (19.5) | 0.22 |
| Dyslipidaemia | 582/946 (61.5) | 6882/12 212 (56.4) | 0.001 |
| Hypertension | 626/1027 (61.0) | 7882/13 170 (59.8) | 0.51 |
| History of ischaemic heart disease | 291/744 (39.1) | 3636/10 398 (35.0) | 0.023 |
| Family history of early CAD | 229/651 (35.2) | 2706/8094 (33.4) | 0.37 |
| Current smoking | 368/1001 (36.8) | 4922/12 920 (38.1) | 0.42 |
| Obesity BMI >30 kg/m2 | 212/913 (23.2) | 2242/11 702 (19.2) | 0.003 |
| Clinical presentation | |||
| Delay symptom onset to admission median IQR 25th, 75th | 280 130, 835 | 230 115, 645 | <0.001 |
| Pain | 898/1062 (84.6) | 11016/13 500 (81.6) | 0.017 |
| Dyspnoea | 256/1035 (24.7) | 3555/12 956 (27.4) | 0.065 |
| Sinus rhythm | 997/1078 (92.5) | 12540/13 803 (90.8) | 0.005 |
| Atrial fibrillation | 481/1078 (4.5) | 727/13 803 (5.3) | 0.005 |
| Heart rate b.p.m., mean ±SD | 76.4 ± 18.2 | 79.0 ± 20.3 | <0.001 |
| Systolic blood pressure mm Hg, mean ±SD | 141.1 ± 25.7 | 135.0 ± 28.4 | <0.001 |
| Diastolic blood pressure mm Hg, mean ±SD | 81.6 ± 16.3 | 79.3 ± 17.9 | <0.001 |
| Killip classes (%) | n = 1081 | n =13810 | <0.001 |
| Class I | 85.9 | 78.7 | |
| Class II | 10.4 | 14.4 | |
| Class III | 2.6 | 3.9 | |
| Class IV | 1.1 | 3.0 | |
| Comorbidities | |||
| Past history of myocardial infarction | 181/1078 (16.8) | 2293/13 656 (16.8) | 1.00 |
| Heart failure NYHA III/IV | 45/1078 (4.2) | 501/13 656 (3.7) | 0.41 |
| Moderate to severe renal disease | 57/1078 (5.3) | 948/13 656 (6.9) | 0.041 |
| Neoplastic disease* | 69/1078 (6.4) | 746/13 656 (5.5) | 0.19 |
| * including malignant neoplasm, leukaemia, lymphoma, metastatic solid tumour | |||
| Table 2Immediate therapy according to the patient’s ECG on admission. | |||
| Immediate pharmacological therapy | |||
| Aspirin | 1014/1083 (93.6) | 13 182/13 828 (95.3) | 0.013 |
| Clopidogrel | 761/1081 (70.4) | 10 089/13 78 (73.2) | 0.046 |
| GP IIb/IIIa antagonist | 244/1071 (22.8) | 4944/13 700 (36.1) | <0.001 |
| UFH | 636/1078 (59.0) | 8936/13 750 (65.0) | <0.001 |
| LMWH | 444/1075 (41.3) | 4815/13 650 (35.3) | <0.001 |
| Beta-blocker | 772/1078 (71.6) | 9551/13 740 (69.5) | 0.16 |
| ACE-inhibitor | 410/1075 (38.1) | 6481/13 688 (47.3) | <0.001 |
| Angiotensin II receptor antagonist | 99/1068 (9.3) | 874/13 577 (6.4) | 0.001 |
| Ca-channel blocker | 95/1075 (8.8) | 888/13 601 (6.5) | 0.004 |
| Nitrate | 634/1075 (59.0) | 7856/13 704 (57.3) | 0.31 |
| Lipid lowering drug | 800/1074 (74.5) | 10440/13 752 (75.9) | 0.30 |
| Interventional therapy | |||
| PCI primary | 484/1082 (44.7) | 8745/13 835 (63.2) | <0.001 |
| Any PCI | 751/1085 (69.2) | 10627/13 872 (76.6) | <0.001 |
| Thrombolysis | 6/1085 (0.6) | 681/13 871 (4.9) | <0.001 |
| CABG | 62/1045 (6.0) | 782/13 489 (5.0) | 0.92 |
| Table 3Early outcome according to the patient’s ECG on admission. | |||
| Complications | |||
| Cardiogenic shock | 24/1076 (2.2) | 666/13 711 (4.9) | <0.001 |
| Cerebrovascular event | 4/1076 (0.4) | 115/13 659 (0.8) | 0.11 |
| Re-infarction | 15/1076 (1.4) | 190/13 701 (1.4) | 1.00 |
| Death | 34/1085 (3.1) | 828/13 872 (6.0) | <0.001 |
| Data are given as number of analysed patients/number of patients without missing data (percentage). | |||
The present study identifies a subgroup of AMI patients who were admitted with a normal/non-specific ECG, had elevated cardiac enzymes and were treated for AMI and discharged with a final diagnosis of AMI. The size of this subgroup is considerable and amounts to 7.3% of all the patients admitted for AMI participating in the study. This rate is comparable with the percentage range of AMI patients with a normal ECG on admission found in earlier studies with similar inclusion criteria, in which the rates vary from 3% to 17% [4, 12–15]. The broad variation in the percentages of normal AMI can be explained by the different criteria defining an ECG pattern as normal/non-specific. This makes comparison between the various studies difficult [16]. In a study by Welch et al. [4], as many as 35.1% of the AMI patients studied belonged to the non-specific group, a rate much higher than in this study simply due to the ECG classification criteria and not to a completely different patient collective.
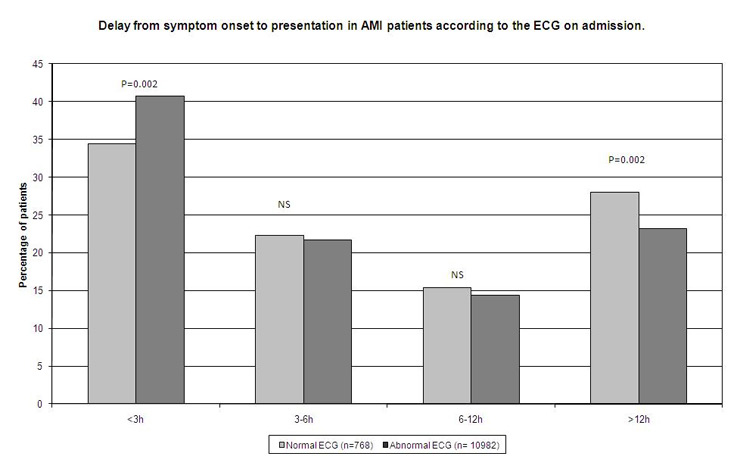
Figure 2
Delay from symptom onset to presentation in AMI patients according to the ECG on admission.
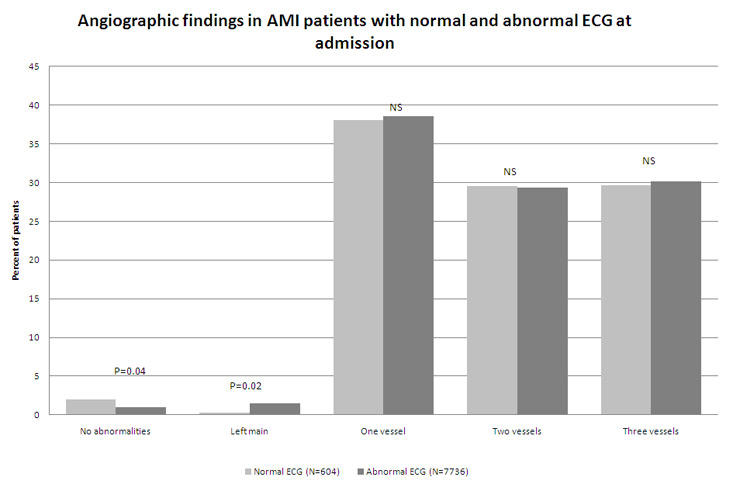
Figure 3
Angiographic findings in AMI patients with normal and abnormal ECG at admission.
Common clinical or demographic characteristics amongst AMI patients with a normal/non-specific ECG could not be identified. Their features and risk factors were very similar to those of the population with an abnormal ECG on admission. These patients also had a more frequent history of ischaemic heart disease which could cause the organism to adapt successfully to its hypoxic condition and therefore show a normal ECG despite AMI and perhaps less typical and acute symptoms. Furthermore, AMI patients presenting with a normal/non-specific ECG were more often obese, which may present technical difficulties in recording the superficial ECG, resulting in a less accurate reading.
Similar studies showed that patients with AMI and a normal ECG on admission were more often male and younger than those with an abnormal ECG [4, 15]. Findings regarding the rates of prior MI varied. Patients with a normal ECG were associated with higher [3] or lower [4, 17] rates of prior AMI; in the present study, however, the rates of prior AMI were the same in both groups.
Despite similar presentation characteristics, the treatment received by patients with a normal/non-specific ECG was less aggressive. This was also the case in a similar study [4] which noted that these patients presented with less typical AMI symptoms and were given their first ECG after a longer delay. In this study procedures were performed after a longer interval after symptom onset. These patients received aspirin, heparin, intravenous beta-blockers or PCI less often but had similar rates of CABG [4]. The differences in care received are not surprising considering the normal ECG findings which are likely to entice clinicians into a diagnosis other than AMI before further examinations have been conducted. In AMI care, time plays a major role and these possible delays may have an impact on the outcome. However, despite the less aggressive treatment, patients in the present study had lower in-hospital mortality rates and a more favourable hospital course regarding cardiogenic shock. Nevertheless, these patients were in a critical situation, since 3.1% died in hospital and several suffered life-threatening complications such as re-infarction and cerebrovascular events as often as those with an abnormal ECG. The 30-day outcome was similar in patients with and without changes on their admission ECG in a study by Welch et al. [4].
Several older studies suggested that in patients with suspected AMI and a normal ECG on admission, the ECG on admission is “better for determining the prognosis than for determining the diagnosis” [5]. The main findings of these studies associate an initial normal/non-specific ECG with a more favourable outcome including less AMI, less life-threatening complications and death [3, 5, 17–19]. Fesmire et al. [20] found there was a 14.2 times greater risk of AMI when the initial ECG was abnormal. Furthermore, the initial ECG as a stratifying tool and was used for separating patients with suspected AMI into low- and high-risk groups for AMI, complications or death, and became an indicator of the ward to which the patient was best suited: ICU; CCU; monitored bed or medical bed. A recent study [4], including only patients with a definite diagnosis of MI, found that patients with AMI and a normal ECG had a 41% lower risk of hospital death. Although it was not significant, there was a similar 42% lower risk of mortality in this study.
Caceres et al. [12] found that all patients with adverse events had ECG changes prior to the event. When changes appear in an initially normal ECG they can be taken as a warning for an adverse outcome and an indicator for taking appropriate action; they can lower expectations of a good prognosis. By following the ECG evolution during hospitalisation with serial ECG readings, adverse events may be dealt with more efficiently.
It seems surprising that such a large proportion of AMI patients present with a normal ECG and the reasons why this reliable diagnostic tool fails in its duty cannot be identified in the patients’ features. The reasons suggested up to now for this are, on the one hand, related to the delay between the time of symptom onset to the time of the first ECG recording or, on the other hand, to the characteristics of the lesion, such as location and size [12].
First, it may be that the patients who have a normal ECG on admission present very early after symptom onset and the organic changes are not yet visible on the ECG reading [5, 17, 21]. In the present study, however, the patients who presented with a normal/non-specific ECG tended to arrive later, with a median time difference of 50 minutes, than those whose initial ECG showed abnormalities. Their first ECG was recorded after a longer delay [4]. Hence it was not possible to correlate the time between the onset of symptoms and the patients’ admission with the probability that the initial ECG would have an abnormal pattern, which is in accordance with findings by Caceres et al. [12].
Following this delay hypothesis, Singer et al. [14] assessed the time that an ECG remained normal after symptom onset. No matter how long an ECG remains normal, it does not rule out AMI. Hence there are organic changes that the ECG cannot detect: a normal ECG could then be associated with a particular type of lesion.
Secondly, lower peak CK levels have been associated with smaller MIs [22] and have also been found frequently in AMI patients presenting with a normal ECG [3, 5, 12, 15, 17, 23]. A minimal infarct size may be required for recognition by a superficial ECG. Ward et al. found that the infarction needs to cover at least 3% of the left ventricle [24].
The final reason for silent electrocardiographic findings in MI may lie in the location of the lesion, which may also be an obstacle to detection by the ECG, since up to 50% of infarctions in the left circumflex distribution may be silent [25], and the extent of the surface ECG’s abnormality depends on the location of the lesion [26–27]. Accordingly, an ECG can overlook a lesion, which explains why 98% of the patients with a normal/non-specific ECG in this study showed abnormal coronary angiographic findings. Zalenski et al. [15] analysed the angiographic findings of a group of patients with a normal initial ECG and associated a normal ECG with a culprit lesion in a peripheral branch.
Deficient in diagnostic evidence, a normal admission ECG in an ischaemic patient may delay the final diagnosis and initiation of treatment, in which absence of a time delay plays a major role in a favourable outcome. The rates of missed diagnoses and inadvertent discharge of AMI patients vary between 2% to 8% of all presenting AMI patients [13] and one of the factors associated with discharge with AMI rather than hospitalisation was a normal ECG [13, 17, 28]. A non-admitted AMI patient had a 1.9 times higher risk of death compared to those admitted [13]. Moreover, the time lapse between presentation and definite diagnosis of AMI was longer in patients with a normal ECG, despite the same presentation time [4, 17], and this may also hold back the start of therapy and worsen the outcome.
Therefore, as long as the diagnosis is accurate and patients are hospitalised and treated accordingly, a normal ECG on admission can be interpreted as a predictor of a better short-term outcome. Recognition of a silent electrocardiographic MI requires all the physician’s attention and clinical skills to ensure the correct diagnosis and the appropriate care. However, to improve diagnosis in coronary care, repeated cardiac marker measurements are needed to strengthen the findings. The latest development in troponin assays [29–30] may, thanks to their higher sensitivity and rapid availability, improve the therapeutic pathway and represent the missing cornerstone for AMI patients.
The limitations encountered are common to all registries. Data are only available on the admission ECG and symptoms; all subsequent ECG readings and symptom evolution were not recorded in the registry and therefore preclude any further analysis. The AMIS registry records coronary angiographic findings located in one or more of the main vessels (one-, two- or three-vessel disease and LCA yes/no) which prevents study of the relationship between peripheral lesions and a normal ECG.
In the present study the ECG readings were not centralised and were undertaken by the hospital physicians on duty. All the patients in this study were admitted with suspected AMI and had indeed a final discharge diagnosis of AMI; the temporal relation between admission ECG and diagnosis was not recorded. The cardiac marker measurements of the patients included were undertaken in their respective hospitals. The technical devices used may diverge and different cut-off values for MI could cause an unwitting bias.
However, the large number of patients analysed added to our understanding of AMI and pointed up the necessity of investigating further diagnostic pathways to rapid identification and risk assessment of patients presenting with symptoms of cardiac ischaemia without the expected ECG changes.
Normal or non-specific ECG changes in patients admitted for suspected AMI do not rule out AMI. Moreover, AMI patients presenting with a normal/non-specific ECG are not uncommon and cannot be categorised by common clinical or demographic features. They are treated less aggressively and after a longer time lapse. Although these patients had lower in-hospital mortality and less frequent cardiogenic shock, they have a risk of re-infarction and cerebrovascular events similar to patients with an abnormal ECG on admission. Further studies are needed to assess whether these particular MI patients could hope for an even more favourable outcome if they received care with the same intensity as those who present with an abnormal ECG, and also to find a diagnostic pathway to rapid identification of AMI when ECG evidence is lacking.
1 Hoekstra J, Cohen M. Management of patients with unstable angina / non-ST-elevation myocardial infarction: a critical review of the 2007 ACC /AHA guidelines. Int J Clin Pract. 2009;63(4):642–55.
2 Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29(23):2909–45.
3 Bell MR, Montarello JK, Steele PM. Does the emergency room electrocardiogram identify patients with suspected myocardial infarction who are at low risk of acute complications? Aust N Z J Med. 1990;20(4):564–9.
4 Welch RD, Zalenski RJ, Frederick PD, Malmgren JA, Compton S, Grzybowski M, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA. 2001;286(16):1977–84.
5 Brush JE, Jr., Brand DA, Acampora D, Chalmer B, Wackers FJ. Use of the initial electrocardiogram to predict in-hospital complications of acute myocardial infarction. N Engl J Med. 1985;312(18):1137–41.
6 Schoenenberger AW, Radovanovic D, Stauffer JC, Windecker S, Urban P, Eberli FR, et al. Age-related differences in the use of guideline-recommended medical and interventional therapies for acute coronary syndromes: a cohort study. J Am Geriatr Soc. 2008;56(3):510–6.
7 Stolt Steiger V, Goy J-J, Stauffer J-C, Radovanovic D, Duvoisin N, Urban P, et al. Significant decrease in in-hospital mortality and major adverse cardiac events in Swiss STEMI patients between 2000 and December 2007. Swiss Med Wkly. 2009;139(31-32):453–7.
8 Jeger RV, Radovanovic D, Hunziker PR, Pfisterer ME, Stauffer JC, Erne P, et al. Ten-year trends in the incidence and treatment of cardiogenic shock. Ann Intern Med. 2008;149(9):618–26.
9 Radovanovic D, Erne P, Urban P, Bertel O, Rickli H, Gaspoz JM. Gender differences in management and outcomes in patients with acute coronary syndromes: results on 20,290 patients from the AMIS Plus Registry. Heart. 2007;93(11):1369–75.
10 Urban P, Radovanovic D, Erne P, Stauffer JC, Pedrazzini G, Windecker S, et al. Impact of changing definitions for myocardial infarction: A report from the AMIS Registry. Am J Med. 2008;121(12):1065–71.
11 Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000;21(18):1502–13.
12 Caceres L, Cooke D, Zalenski R, Rydman R, Lakier JB. Myocardial infarction with an initially normal electrocardiogram – angiographic findings. Clin Cardiol. 1995;18(10):563–8.
13 Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342(16):1163–70.
14 Singer AJ, Brogan GX, Valentine SM, McCuskey C, Khan S, Hollander JE. Effect of duration from symptom onset on the negative predictive value of a normal ECG for exclusion of acute myocardial infarction. Ann Emerg Med. 1997;29(5):575–9.
15 Zalenski RJ, Rydman RJ, Sloan EP, Caceres L, Murphy DG, Cooke D. The emergency department electrocardiogram and hospital complications in myocardial infarction patients. Acad Emerg Med. 1996;3(4):318–25.
16 Hollander JE. Risk stratification of emergency department patients with chest pain: the need for standardized reporting guidelines. Ann Emerg Med. 2004;43(1):68–70.
17 Rouan GW, Lee TH, Cook EF, Brand DA, Weisberg MC, Goldman L. Clinical characteristics and outcome of acute myocardial infarction in patients with initially normal or nonspecific electrocardiograms (a report from the Multicenter Chest Pain Study). Am J Cardiol. 1989;64(18):1087–92.
18 Forest RS, Shofer FS, Sease KL, Hollander JE. Assessment of the standardized reporting guidelines ECG classification system: the presenting ECG predicts 30-day outcomes. Ann Emerg Med. 2004;44(3):206–12.
19 Stark ME, Vacek JL. The initial electrocardiogram during admission for myocardial infarction. Use as a predictor of clinical course and facility utilization. Arch Intern Med. 1987;147(5):843–6.
20 Fesmire FM, Percy RF, Wears RL, MacMath TL. Risk stratification according to the initial electrocardiogram in patients with suspected acute myocardial infarction. Arch Intern Med. 1989;149(6):1294–7.
21 McGuinness JB, Begg TB, Semple T. First electrocardiogram in recent myocardial infarction. Br Med J. 1976;2(6033):449–51.
22 Kawaguchi K, Sone T, Tsuboi H, Sassa H, Okumura K, Hashimoto H, et al. Quantitative estimation of infarct size by simultaneous dual radionuclide single photon emission computed tomography: comparison with peak serum creatine kinase activity. Am Heart J. 1991;121(5):1353–60.
23 Slater DK, Hlatky MA, Mark DB, Harrell FE, Jr., Pryor DB, Califf RM. Outcome in suspected acute myocardial infarction with normal or minimally abnormal admission electrocardiographic findings. Am J Cardiol. 1987;60(10):766–70.
24 Ward RM, Ideker RE, Wagner GS, Alonso DR, Bishop SP, Bloor KA, et al. Myocardial infarcts in the lateral third of the left ventricle, size and ECG recognition. Am J Cardiol. 1980;13(Abstract):478.
25 Blanke H, Cohen M, Schlueter GU, Karsch KR, Rentrop KP. Electrocardiographic and coronary arteriographic correlations during acute myocardial infarction. Am J Cardiol. 1984;54(3):249–55.
26 Berry C, Zalewski A, Kovach R, Savage M, Goldberg S. Surface electrocardiogram in the detection of transmural myocardial ischemia during coronary artery occlusion. Am J Cardiol. 1989;63(1):21–6.
27 Huey BL, Beller GA, Kaiser DL, Gibson RS. A comprehensive analysis of myocardial infarction due to left circumflex artery occlusion: comparison with infarction due to right coronary artery and left anterior descending artery occlusion. J Am Coll Cardiol. 1988;12(5):1156–66.
28 Lee TH, Cook EF, Weisberg M, Sargent RK, Wilson C, Goldman L. Acute chest pain in the emergency room. Identification and examination of low-risk patients. Arch Intern Med. 1985;145(1):65–9.
29 Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med. 2009;361(9):868–77.
30 Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361(9):858–67.
Main sponsors: Astra-Zeneca, Bayer-Schering, Biotronik, Daiichi-Sankyo/Lilly, Invatec, A. Menarini, Medtronic, St. Jude Medical, all in Switzerland. Donators: Abbott, Biosensors, Bristol-Myers Squibb, GlaxoSmithKline, Johnson & Johnson, Merck Sharp & Dohme-Chibret, Essex, Novartis, Pfizer, sanofi-aventis, Servier, SPSS and Takeda, all in Switzerland.