Bilateral total knee arthroplasty in a patient with haemophilia A, high inhibitor titre and aneurysma spurium of the popliteal artery
DOI: https://doi.org/10.4414/smw.2010.13094
R
Harstall, J
Kajahn, S
Anderson, S
Eggli, LH
Frauchiger
Summary
The authors report on bilateral simultaneous knee arthroplasty in a 40-year-old male patient with haemophilia A, high inhibitor titre and an aneurysma spurium of the right popliteal artery. Both knees showed a fixed flexion deformity of 20 degrees. To build up haemostasis, treatment with activated prothrombin complex concentrate (APCC) and recombinant activated factor seven (rFVIIa) was initiated preoperatively. A tourniquet was used on both sides during the operation and factor VIII (FVIII) was administered to further correct coagulopathy. On the eleventh postoperative day the patient complained of increasing pain and pressure in the right knee. An ultrasound suggested aneurysm, which was confirmed by substraction angiography. Under the protection of rFVIIa the aneurysm could be coiled and further rehabilitation was uneventful. At one year post-op the patient presented a range of motion of 90/5/0° for both knees and had returned to full time office work. This case indicates that haemophiliacs with high antibody titre and destruction of both knees can be operated on in one session in order to diminish the operative risk of two consecutive surgical procedures, thus allowing an effective rehabilitation programme. Because of the significant frequency of popliteal aneurysms, preoperative angiography is recommended.
Introduction
Hemophilia A is an X-linked genetic haemorrhagic disorder characterised by the absence of clotting factor VIII (FVIII). One in 10 000 males is born with deficiency of FVIII molecules [1]. Haemophiliacs suffer from major arthropathy, mainly of the hip, knee and ankle. Joints are exposed to repetitive intraarticular bleeding, leading to cartilage destruction, pain and limited range of motion [2–6]. Recurrent haemarthros is treated with prophylactic donation of coagulation factors, puncture, open synovectomy or radiosynorthesis [4, 5, 7]. In most cases the natural course of this disease ends in complete destruction of the joint and ankylosis, with complete loss of function [2, 8]. Usually the bleeding tendency can be corrected by substitution of FVIII concentrates. However, up to 25% of all patients with haemophilia A develop inhibitors that neutralise the substituted FVIII [9]. Inhibitors are usually IgG antibodies divided into two different entities (type I/II) depending on high or low rise of titre after FVIII substitution [1]. The difficulties for haemophiliacs with inhibitors are i) to keep the inhibitor development controlled, ii) the higher incidence of joint and muscle bleeds and their complications, and iii) the higher morbidity during surgery because of the challenging pharmacological treatment. Thus, when contemplating surgery in haemophiliacs with high inhibitor titre, two factors – restricted quality of life and major surgical risks – must be weighed against each other [2, 3]. Also, high costs for the healthcare system must be taken into account.
In this article the authors report on bilateral total knee arthroplasty (TKA) in a 40-year-old haemophilia A patient with immobilising destructive knee arthritis. The surgical intervention, performed as a bilateral TKA in one session, the medication strategy, complications with a popliteal aneurysm, cost and the outcome of surgery are discussed.
Case description
The patient was a 40-year-old male with severe haemophilia A (factor VIII: C< 1%) and high responding inhibitors. The genetic mutation for the haemophilia A could not be identified, but an intron 22 inversion, which is commonly seen with severe haemophilia A with high responding inhibitors, was excluded. The patient had been treated since childhood in a haemophilia centre for haemorrhagic episodes using activated prothrombin complex concentrate (APCC) which activates factor X directly and bypasses the inhibitor-induced block (factor VIII inhibitor bypassing agent, FEIBA VH, Baxter AG, Deerfield, IL, USA), porcine factor VIII ([pFVIII], Hyate C®, Opopharma, Glattbrugg, Switzerland) and for the previous two years with recombinant activated factor VII ([rFVIIa], NovoSeven®, Novo Nordisk Pharma AG, Princeton, NJ, USA). Through blood transfusions the patient had become infected with hepatitis B and C but showed no indications of liver cirrhosis.
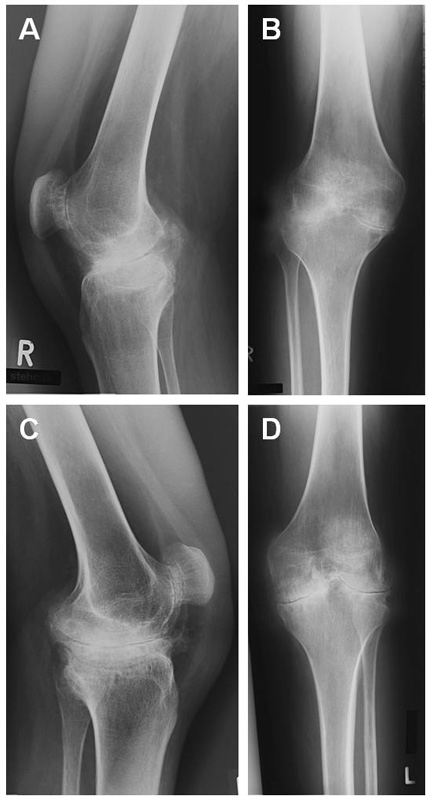
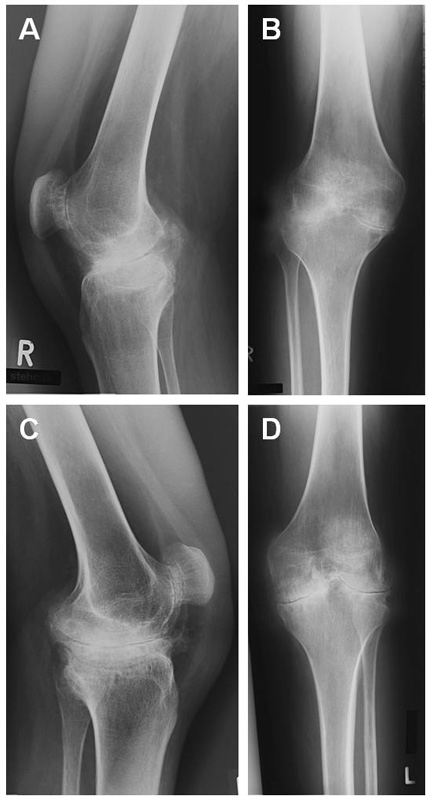
Figure 1
Preoperative x-rays of both knees. Arthrotic deformities in all three compartments of the knee joints could be observed. (a) Right knee lateral view (b) Right knee anterior-posterior view (c) Left knee lateral view (d) Left knee anterior-posterior view.
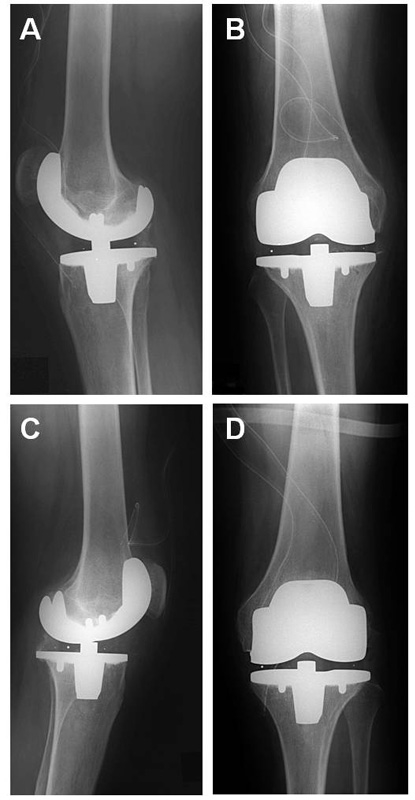
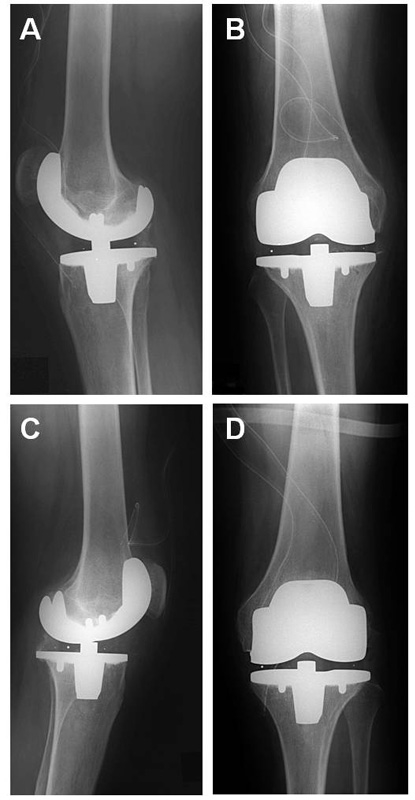
Figure 2
X-rays of both knees after surgical implantation of prostheses. (a) Right knee lateral view (b) Right knee anterior-posterior view (c) Left knee lateral view (d) Left knee anterior-posterior view.
Recurrent joint haemorrhaging led to severe haemophiliac arthropathy involving knees, elbows and ankle joints. Persistent haemorrhaging and associated secondary degenerative disease led to a severe bilateral fixed knee flexion deformity of some 20° associated with severe pain and progressive difficulty in walking (fig. 1). The patient was hardly able to rise from a seated position.
After careful evaluation the authors were convinced that the possible benefit of a bilateral knee joint replacement outweighed the risks and therefore decided to perform this intervention in close cooperation with the haematological specialists.
Operative procedure
The patient was hospitalised four days before the operation. Responding inhibitor activity level was high, measured as 2 Bethesda units (standard value is supposed to be negative). A Mahourkar catheter was inserted for delivery of extracorporeal immunoabsorption treatment and rFVIIa (120 μg/kg body weight) was administered. Additionally, APCC was given on day 1 and day 3 before the operation with each 6000 IU. On the basis of this treatment there was no elevated inhibitor titre on the day of the operation. Thus, 100 IU/kg body weight of factor VIII ([FVIII], Haemate HS Aventis ZLB Behring®, King of Prussia, PA, USA) was given for the operation. After reaching a normal aPTT (activated partial thromboplastin time) bilateral simultaneous total knee arthroplasty was performed under general anaesthesia, starting on the right side. The right knee was technically more demanding and clinically more symptomatic. Tourniquet time for the right knee was 103 minutes and for the left knee 115 minutes. The surgery was performed using a midline incision with medial parapatellar arthrotomy. To mobilise the knees extensive adhesiolysis of the dorsal capsule and the collateral ligaments had to be performed. The course of surgery was uneventful with no major bleeding occurring. Estimated blood loss amounted to 1000 mL for each procedure. Both components (femoral and tibial) were cemented with an ultra congruent tibial polyethylene plateau sacrificing the posterior cruciate ligaments (Innex® Sulzer AG, Baar, Switzerland). After implantation the passive range of motion was 80-5-0° (flexion/extension) for both knees, with a soft endpoint in extension. Before closing the wound the tourniquet was opened and meticulous inspection of the surgical area was performed to detect minor bleeding sources (fig. 2).
Within three days postoperatively thrombotic prophylaxis was performed with subcutaneous low molecular weight heparin for the period that FVIII substitution (10 000 IU) was performed. On postoperative day 4, since the aPTT value was prolonged and the rise in factor VIIIC poor, a rise in the responding inhibitor titre occurred. On the fifth and seventh postoperative days APCC was therefore administered again, but without change of the aPTT to normal range. For this reason the treatment was changed to rFVIIa 120 μg/kg body weight, administered every three hours. Nevertheless, haemorrhage into the right knee joint occurred and on the sixth postoperative day into the left knee joint. Fortunately the patient did not suffer major pain and clinical examination of both knees still showed tender soft tissue. The skin was slightly under tension. After the therapy with rFVIIa was increased the haemorrhage stopped and the clinical signs of haemorrhage diminished.
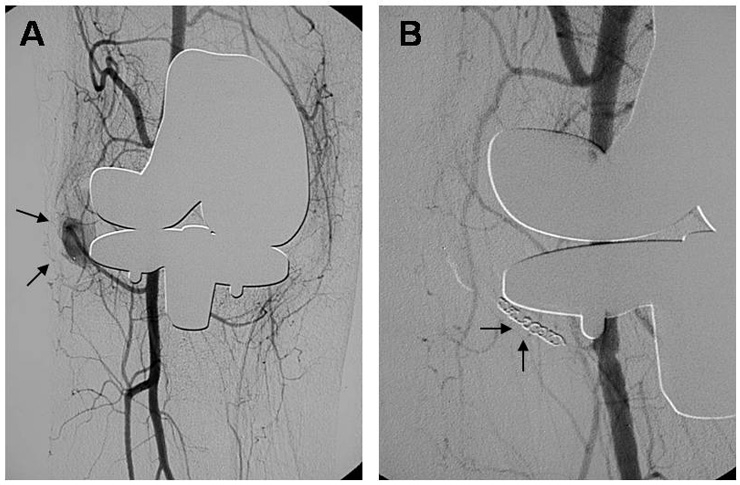
On the eleventh postoperative day the patient complained of new and severe pain in the right knee. Ultrasound with duplex colour Doppler suggested the diagnosis of false aneurysm. Digital subtraction angiography (DSA) showed a false aneurysm arising from the inferior medial genicular artery into the knee joint (fig. 3). The morphology of the vascular appearance suggested a pseudoaneurysm formation with irregular saccular form dilatation of the artery. Irregularities of the adjacent synovial arterial vessels were also evident. Under protection of rFVIIa embolisation was performed successfully with no additional complication.
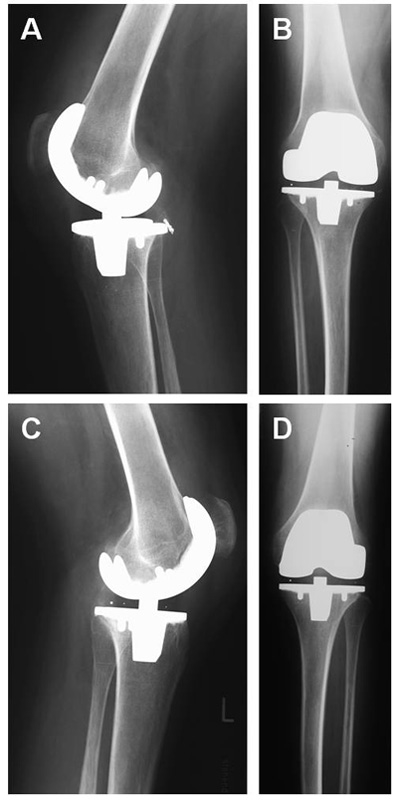
Thereafter the patient could be mobilised with crutches and left the hospital on day 26. One year after the operation the patient reached a bilateral flexion of 90° passively and up to 80° actively with a persistent extension deficit of 5°. He was able to walk continuously without assistance for up to three hours, and rising from a chair posed no further problem. X-rays showed no signs of loosening (fig. 4).
The total cost of the treatment, including the costs of total knee replacement, FVIII 59.000 IU and rFVIIa 1464 mg, was over CHF 1 million.
Discussion
Total knee replacement for haemophilic patients is generally associated with significant improvement of walking capacity and range of motion [3, 10–13], despite the higher risk of postoperative haemorrhage, nerve palsy, skin necrosis and infection [3, 14]. In the case of bilateral destruction of the knee joints simultaneous bilateral implantation of the prostheses is recommended in haemophiliacs [15]. This is because the cumulative perioperative risks of two consecutive surgical procedures are significantly higher. Substantial blood loss and complex haemostatic control maintained for extended time periods to facilitate wound healing and physiotherapy have to be risked twice. However, bilateral TKA comprises the same if not as severe risks due to the prolonged operation time. Nonetheless, experience of bilateral TKA has shown that the ultimate functional outcome is improved [16]. The flexion deformity and decreased walking capacity in haemophiliac knee arthropathy can be treated more easily if both knees can be mobilised simultaneously during rehabilitation [8, 10–12]. Also, the high cost of bypassing therapy can if necessary be kept lower [16].
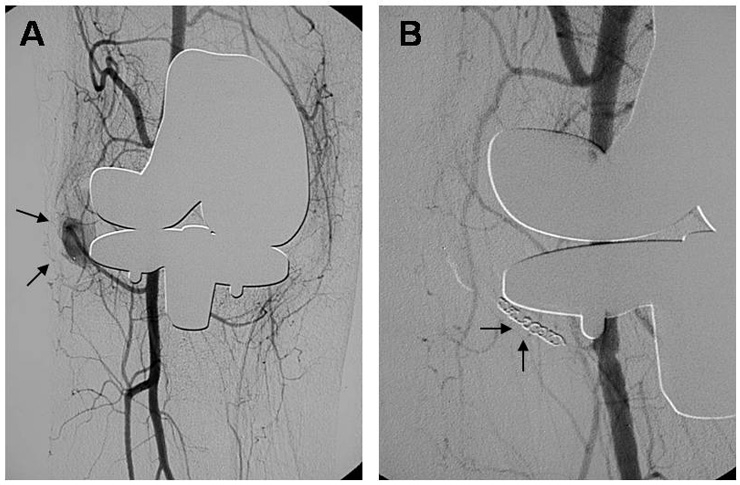
Figure 3
Angiographic photographs showing a false aneurysm of the inferior medial popliteal artery of the right knee (a) before and after intervention via coiling (b).
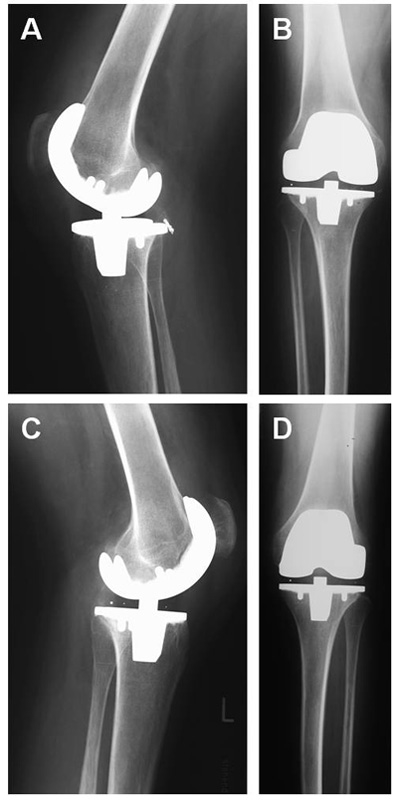
Figure 4
One year postoperative x-rays of both knees. Correct anatomic position of the prostheses, no signs of loosening. (a) Right knee lateral view (b) Right knee anterior-posterior view (c) Left knee lateral view (d) Left knee anterior-posterior view.
Some authors report a fair gain in range of motion postoperatively in haemophilic arthropathy [17, 18]. In the case presented the extensive debridement and release, especially of the posterior knee compartment, resulted in an intraoperative range of motion of flexion/extension 80/5/0° with soft endpoints. Due to an intensive postoperative rehabilitation programme this range of motion could be maintained and remained the same for one year after surgery. The lasting gain in range of motion was impressive considering the preoperative fixed flexion deformity of 20°.
Before the introduction of FVIIa and inhibitor bypassing agents such as APCC, total joint replacement in patients with haemophilia A and high inhibitor titre was risky or even impossible [19]. With its introduction in 1988, total knee replacement became possible for these patients [20] with acceptable clinical results [3, 10–13]. With treatment by recombinant products the patients benefit from effective haemostasis with no significant rise in inhibitor levels [21, 22]. In our case we did not substitute FVIII preoperatively so as to avoid boosting the inhibitors. The patient was treated with FVIII directly before the operation and surgery was started after reaching normal levels of aPTT. After the surgery substitution with FVIII was continued. During postoperative mobilisation and rehabilitation rFVIIa was administered again. Altogether the complex treatment with factors and agents led to an acceptable control of bleeding. We therefore suggest closeknit supervision of haemostatic parameters by all medical personnel involved.
Saris et al. [23] described non-traumatic aneurysms of the knee in seven out of ten cases with haemophilia in TKA. Rodriguez-Merchan found one out of 36 haemophilic arthropathies with a pseudoaneurysm of a geniculate artery treated successfully by embolisation [24]. Recently Sloan et al. and Gupta et al. presented cases of endovascular treatment for traumatic popliteal artery pseudoaneurysms after TKA [25, 26]. A possible mechanism for preoperative formation of a false aneurysm could be repetitive mechanical damage to the vessels by the arthritic changed joint (osteophytes, scarring), in combination with a decreased healing capacity of the vascular wall. In the case presented operative damage to the inferior medial popliteal artery as the cause for formation of the aneurysm cannot be excluded. The medial genicular artery is at risk because of its course along the medial joint line, particularly when the surgeon exposes the medial side of the knee [27]. Hence exact knowledge of the location of vascular structures adjacent to the surgical field is essential to prevent injuries [28]. Typically, bleeding due to the false aneurysm started with a delay of 11 days and was marked by an increased feeling of intraarticular pressure and inability to flex.
As a fast screening method ultrasound with duplex colour Doppler was performed and suggested the formation of a false aneurysm. As suggested by Mann et al. [29], the authors performed a DSA clearly revealing a false aneurysm arising from the inferior medial genicular artery, and obtained rapid embolisation using metal coils [30]. With the knowledge of this case, the authors suggest that angiography before implantation of a total knee prosthesis in haemophilic arthropathy could be performed routinely [23, 27, 28]. If sudden pain in the knee occurs after TKA one should bear in mind possible false aneurysm formation or other vascular complications.
The high cost of the procedure (over CHF one million) must be weighed against the costs incurred by immobilisation of the patient. These would include probable unemployment due to disability and the cost of hiring professional caregivers to assist in daily living. With both knees functioning to a satisfactory level our patient not only raised his quality of life but was fully able to return to normal office work. There have been several publications of TKA in haemophiliacs with high inhibitor titres and vascular complications [21–24]. Nonetheless, to the best of the authors’ knowledge no case has been described of bilateral TKA operated on in one session with detailed coagulation management as here presented. Also, the complication of a false aneurysm and its therapeutic intervention after TKA in haemophiliacs has not been presented as it is herein.
Conclusion
Given the specific treatment of a haemophiliac with a high antibody titre presented here, the authors would like to suggest that in the light of this case surgeons should consider operating on destroyed knees in one session. As was shown here, this approach may reduce operative risks and allows effective rehabilitation.
Treatment with rFVIIa and APCC to control perioperative bleeding for the implantation of total knee prostheses is considered a safe solution for patients with haemophilia and a high inhibition titre. According to the available literature on the significant frequency of popliteal aneurysms in hemophiliacs, preoperative angiography or other diagnostics for the detection of vascular complications are recommended.
Correspondence:
Roger Harstall
Department of Orthopaedic Surgery and Traumatology
Buergerspital
CH-4500 Solothurn
Switzerland
roger.harstall@gmx.net
References
1 Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison’s principles of internal medicine. 16th ed. USA: McGraw-Hill; 2005.
2 Legroux-Gerot I, Strouk G, Parquet A, Goodemand J, Gougeon F, Duquesnoy B. Total knee arthroplasty in hemophilic arthropathy. Joint Bone Spine. 2003;70(1):22–32.
3 Norian JM, Ries MD, Karp S, Hambleton J. Total knee arthroplasty in hemophilic arthropathy. J Bone Joint Surg Am. 2002;84-A(7):1138–41.
4 Nilsson IM, Berntorp E, Lofqvist T, Pettersson H. Twenty-five years’ experience of prophylactic treatment in severe haemophilia A and B. J Intern Med. 1992;232(1):25–32.
5 Ribbans WJ, Giangrande P, Beeton K. Conservative treatment of hemarthrosis for prevention of hemophilic synovitis. Clin Orthop Relat Res. 1997;343:12–8.
6 Rodriguez-Merchan EC, Magallon M, Galindo E, Lopez-Cabarcos C. Hemophilic synovitis of the knee and the elbow. Clin Orthop Relat Res. 1997;343:47–53.
7 Gilbert MS, Radomisli TE. Therapeutic options in the management of hemophilic synovitis. Clin Orthop Relat Res. 1997;343:88–92.
8 Luck JV Jr, Kasper CK. Surgical management of advanced hemophilic arthropathy. An overview of 20 years’ experience. Clin Orthop Relat Res. 1989;242:60–82.
9 Gouw SM and van den Berg, HM. The multifactorial etiology of inhibitor development in hemophilia: genetics and environment. Semin Thromb Hemost. 2009; 35(8):723–34
10 Fehily M, Fleming P, O’Shea E, Smith O, Smyth H. Total knee arthroplasty in patients with severe haemophilia. Int Orthop. 2002;26(2):89–91.
11 Goddard NJ, Rodriguez-Merchan EC, Wiedel JD. Total knee replacement in haemophilia. Haemophilia. 2002;8(3):382–6.
12 Goldberg VM, Heiple KG, Ratnoff OD, Kurczynski E, Arvan G. Total knee arthroplasty in classic hemophilia. J Bone Joint Surg Am. 1981;63(5):695–701.
13 Lachiewicz PF, Inglis AE, Insall JN, Sculco TP, Hilgartner MW, Bussel JB. Total knee arthroplasty in hemophilia. J Bone Joint Surg Am. 1985;67(9):1361–6.
14 Solimeno LP, Manusco ME, Pasta G, Santagostino E, Perfetto S, Mannucci PM. Factors influencing the long-term outcome of primary total knee replacement in haemophiliacs: a review of 116 procedures at a single institution. Br J Haematol. 2009;145(2):227–34.
15 Reichel H, Birke A, Wolf HH. Knieendoprothetik bei hämophiler Arthropathie: Ergebnisse, Probleme und Komplikationen. Z Orthop Ihre Grenzgeb. 2001;139(2):120–6.
16 Teitel JM, Carcao M, Lillicrap D, Mulder K, Rivard GE, St-Louis J, et al. Orthopaedic surgery in haemophilia patients with inhibitors: a practical guide to haemostatic, surgical and rehabilitative care. Haemophilia. 2009;15:227–39.
17 Luck JV Jr. Surgical management of advanced hemophilic arthropathy. Prog Clin Biol Res. 1990;324:241–56.
18 Rodriguez-Merchan EC, Magallon M, Galindo E. Joint debridement for haemophilic arthropathy of the knee. Int Orthop. 1994;18(3):135–8.
19 Rodriguez-Merchan EC. Chirurgische Behandlungsprinzipien bei Hämophiliepatienten. Unfallchirurg. 2003;106(4):264–71.
20 Vermylen J, Peerlinck K. Optimal care of inhibitor patients during surgery. Eur J Haematol Suppl. 1998;63:15–7.
21 Faradji A, Bonnomet F, Lecocq J, Grunebaum L, Desprez D, Kern O, Barbier L, Sibilia J. Knee joint arthroplasty in a patient with haemophilia A and high inhibitor titre using recombinant factor VIIa (NovoSeven): a new case report and review of the literature. Haemophilia. 2001;7(3):321–6.
22 Ilg A, Stahlschmidt K, Zotz RB, Krauspe R, Scharf RE, Gerhardt A. Interdisciplinary management of total knee replacement in a haemophilia patient with high-titre inhibitor and severe arthropathy complicated by an aneurysmatic bone cyst. Haemophilia. 2009;15:377–9.
23 Saris DB, van Rinsum AC, Dhert WJ, Roosendaal G, Mali WP. Periarticular aneurysm formation in haemophilia. Lancet. 1997;15;349(9054):766–8.
24 Rodriguez-Merchan EC. Total knee replacement in haemophilic arthropathy. J Bone Joint Surg Br. 2007;89(2):186–8.
25 Sloan K, Mofidi R, Nagy J, Flett MM, Chakraverty S. Endovascular treatment for traumatic popliteal artery pseudoaneurysms after knee arthroplasty. Vasc Endovasculo Surg. 2009;43(3):286–90.
26 Gupta R, Chitre A, Ryan W. False aneurysm of the anterior tibial artery following total knee arthroplasty. Acta Orthop Belg. 2008;74(1):128–31.
27 Manning MP, Marshall JH. Aneurysm after arthroscopy. J Bone Joint Surg Br. 1987;69(1):151.
28 Stanley D, Cumberland DC, Elson RA. Embolisation for aneurysm after knee replacement: brief report. J Bone Joint Surg Br. 1989;71(1):138.
29 Mann HA, Goddard NJ, Lee CA, Brown SA. Periarticular aneurysm following total knee replacement in hemophilic arthropathy. A case report. J Bone Joint Surg Am. 2003;85-A(12):2437–40.
30 Kickuth R, Anderson S, Peter-Salonen K, Lämmle B, Eggli S, Triller J. Hemophilia A Pseudoaneurysm in a Patient with High Responding Inhibitors Complicating Total Knee Arthroplasty: Embolization: A Cost-Reducing Alternative to Medical Therapy. Cardiovasc Intervent Radiol. 2006;29(6):1132–5.