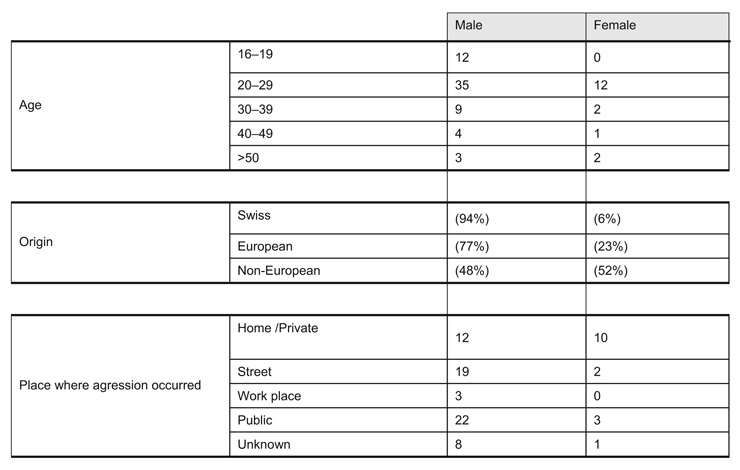
Figure 1
Distribution of ages, origin of patients and places where aggression occurred according to gender, in our cohort of 80 consecutive cases of stab injuries.
DOI: https://doi.org/10.4414/smw.2010.13058
The prevalence of interpersonal violence and related mortality is highly variable around the world [1]. This makes general management rules difficult to establish, especially for regions where those injuries are relatively rare. As an example of this difference, penetrating trauma accounts for up to 80% of all emergency surgical operations performed in South Africa [2], while this is extremely rare in Switzerland. The incidence of homicides has a great variability throughout the world ranging from 0.07 to 141 per 100000 inhabitants per year [3, 4]. Despite these huge differences, the incidence of interpersonal violence is unfortunately prone to increase in many countries and has increased two-fold in Switzerland during the last 10 years [1]. This increase seems to be observed in other European countries [3] and is confirmed by Exadaktylos et al. in a similar setting in Switzerland with an increasing number of hospitalisations due to head trauma casualties [5]. The published studies deal mainly with patient stabilisation [6–10], emergency investigations [11–13] and specific treatment strategies [13–18]. The characteristics of the patients themselves and violence-linked morbidities are rarely analysed.
The aim of the present study was to describe and assess the population of patients admitted to our Emergency department (ED) because of a non-firearm penetrating trauma. We particularly addressed the circumstances and characteristics of the patients and their observed injuries. The medical procedures to manage these stab-wounds were also assessed.
The study took place in a 1300 bed university teaching hospital, with primary and tertiary care. All consecutive adult patients admitted to our ED with a non-firearm, intentional, penetrating trauma occurring between March 2005 and February 2007 were eligible to be included in the study. Non-firearm penetrating trauma was defined as any injury due to any kind of sharp object. Auto-inflicted injuries and non-intentional injuries were excluded as revealed by patient’s history. The ED physicians in charge of the patients completed the standardised data sheets. They were anonymised and pooled in a computerised database (Microsoft Excel). Considering the type of data collected as a detailed medical history, no formal consent was required. According to local prescriptions on observational studies, all of the patients admitted in the ED were informed of the possibility that their medical history may be used for quality control and academic research. The protocol was approved by the Clinical Research Ethics Committee of the University of Lausanne.
To be precisely identified, various types of sharp objects were recorded based on a visual standardised table. Demographics included age, gender, civil and professional status (working vs unemployed) as well as nationality, classified as Swiss, European or non-European. The circumstances of the aggression were specified with 4 items: 1) Place where the aggression occurred, 2) Relationship between the aggressor and the victim, 3) Number of aggressors, 4) Nature of violence. The modality of arrival to the hospital, the potential medical pre-hospital care and the need for initial resuscitation were also noted.
For patients who needed to be hospitalised, the Injury Severity Score (ISS) at admission, the Glasgow Coma Scale (GCS), the type of operation (if performed), the potential need for re-operation, the length of stay (LOS) in the intensive care unit (ICU), the mortality during the initial hospital stay, the overall LOS and the need for re-hospitalisation in our institution were collected. A surgical treatment was considered as therapeutic if a total or partial organectomy was needed, if a surgical manoeuvre was performed to close a laceration or to stop the bleeding, or if a surgical reconstruction was needed to restore the anatomy.
According to institutional guidelines, patients sustaining penetrating trauma to the torso, to the neck or exhibiting any type of respiratory, circulatory or neurological distress were admitted to the resuscitation room. The primary survey was performed according to the recommendations of the Advanced Trauma Life Support (ATLS®) [25]. Focused assessment sonography for trauma (FAST) was performed for unstable patients, and CT scan was indicated according to the clinical findings for stable patients. A local diagnostic exploration of thoracic and abdominal wounds was the choice for a conservative treatment. The investigation plan and initial treatment was determined by the attending surgeon in charge and was based on clinical findings.
This study was prospective, observational and based on multivariate analysis. We particularly compared the demographics of patients admitted for non-firearm intentional penetrating trauma and those of patients admitted to the surgical ward of our ED for other reasons. Similarly, the day and the time of admission were compared to those of general surgical casualties. We also assessed the relationship between the anatomical distribution of injuries and the type of treatment applied (operative, conservative, with or without hospitalisation). The number of injuries inflicted was correlated to the type of weapon. Demographic data of the studied population, circumstances of the aggression and observed injuries were collected. The type of medical care was analysed in relation to the type and severity of injuries.
During the 23 month-period of the study, 37429 patients were admitted to the ED surgical ward. Eighty adult patients (0.2%) admitted to the ED for intentional stab wounds were included during the study period. Young people (mean age 30 / range 16–60) and males (sex ratio 4:1) were over-represented (p <0.001) in this population. Distribution of age, gender and places where the aggression occurred is summarised in figure 1. A total of 61% of these patients belonged to the 20–30 year age group.
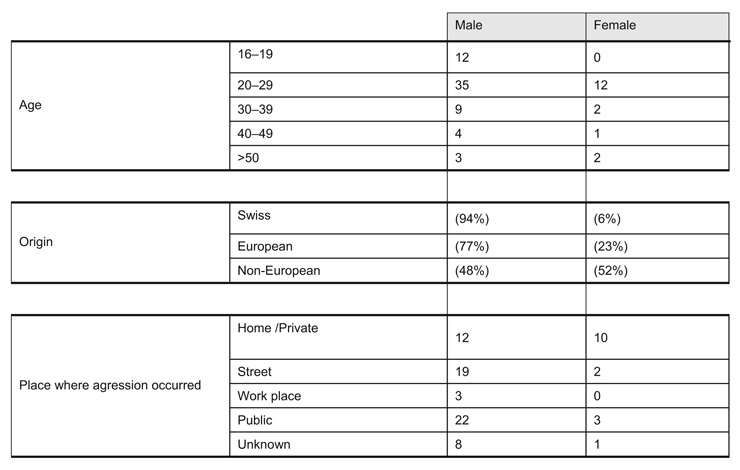
Figure 1
Distribution of ages, origin of patients and places where aggression occurred according to gender, in our cohort of 80 consecutive cases of stab injuries.
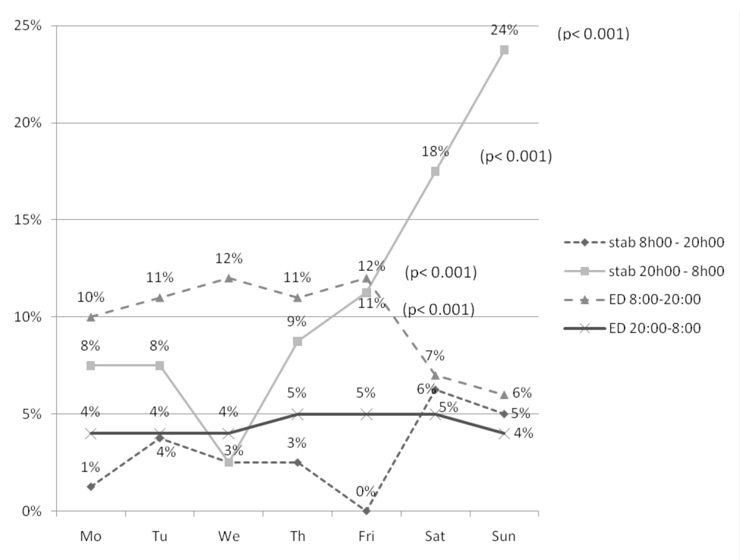
Figure 2
Chronologic distribution of the surgical ED admissions: Penetrating trauma (stab) is over-represented at night on Friday, Saturday and Sunday when compared to the other surgical casualties (ED) (p <0.001).
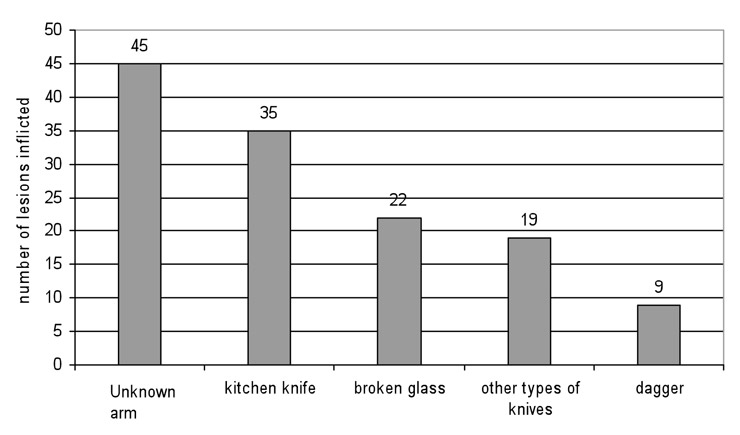
Figure 3
Number of injuries inflicted according to the type of weapon, in our cohort of 80 consecutive stab injuries.
Nationality was reported in 70 patients (87.5%). When compared to the general population living in Switzerland [1], foreigners were significantly overrepresented in our series of patients admitted for intentional stab wounds (38 [54%], p <0.001). Among them, 31 were non-European Union patients and 26 (68%) originated from a continent other than Europe. Moreover, 11 women out of 13 (85%) were foreigners. Unemployment was reported for 40 patients (50%) and was overrepresented in our series when compared to the official Swiss statistics (p <0.001).
Patients in our series differed significantly from the general population of patients admitted to our ED in two aspects. As shown in figure 2, 63% of patients were admitted on the last three days of the week (Friday to Sunday) (p <0.001). These patients were mainly admitted during night time (8pm – 8am) (p <0.001) (overall day: night ratio 2:8). The violence occurred almost equally in the private victim’s sphere, or on the street and in other public places like bars, discotheques or restaurants (27%, 27% and 31% respectively, figure 1). In contrast to men (19%), 63% of women were wounded in a generally private context.
When the type of weapon was defined, it was found that 63% of injuries were inflicted by knives. The localisations of the injuries inflicted by knives are listed in table 1. When the type of weapon could not be defined (26%), the violence occurred on the street or in a public place in 62% of cases. Broken glass or bottles were reported in 15 cases (66%), essentially in public places (figure 3). A total of 48 patients (60%) were assaulted by an unknown individual according to the victims, and 21 assaults (26%) occurred in a context of domestic violence.
Nearly half of patients (n = 38/48%) came by themselves, including 2 patients who had sustained an injury to the abdomen and one patient with an injury to the thorax. Thirty-three (41%) patients were transported by an ambulance or a rescue helicopter staffed with an emergency physician. The ways used to reach the ED are described in figure 4. There was no correlation between the type of pre-hospital transportation and the severity of injuries.
Fourteen patients (18%) required initial admission to the resuscitation room. Ten patients (15%) required a surgical treatment. A laparoscopy was performed in 4 cases (5%) with the main intention to check the integrity of the parietal anterior peritoneum. In two cases, a peritoneal injury required a laparotomy, of which one was therapeutic. The mean ISS of patients requiring surgery was 10 (range 4–20). The mean operative time was 79 min (range 15 min – 162 min). The Cell Saver® was used in two cases and allowed retransfusion of 775 and 770 ml of blood respectively. No additional blood products were administered to these patients. The other requirements for blood products in this series were two units of fresh frozen plasmas administered to one patient, and one unit of packed red cells to another. Only one re-operation out of ten (10%) was needed on day 5 because of a duodenal perforation missed during the initial operative intervention. The mean overall length of stay was 5.5 days (1–15) including 2 days in ICU for two patients. No patient died in the present series.
Out of the 66 patients (83%) treated on an ambulatory basis, 21 (25%) sustained multiple stab wounds. Thirty-four patients (43%) sustained head and neck trauma, the majority of which were superficial lesions of the scalp treated by simple sutures under local anaesthesia. Thirty (38%) patients sustained thoracic, or abdominal injuries or a combination of these. Limbs were injured in 15 cases (19%). Of these, 45 patients (74%) could be discharged the same day. The only patient whose thoracic lesion was operatively treated had a thoraco-abdominal injury actively bleeding from a liver laceration (abdominal AIS = 4; chest AIS = 1). The positive operative findings were a hepatic laceration, a duodenal and a multi-focal jejunal laceration. None of the limb injuries were complicated with vascular or nervous injury. The regional distribution of the lesions and the type of their management is described in the figure 5.
| Table 1Distribution of injuries inflicted by knives. | |
| Upper limb | 15 (33%) |
| Abdomen | 7 (16%) |
| Thorax | 9 (20%) |
| Face | 6 (13%) |
| Head | 3 (7%) |
| Neck | 3 (7%) |
| Lower limb | 2 (4%) |
| TOTAL | 45 (100%) |
Despite the fact that our study demonstrates that stab wounds remain rare in Switzerland, accounting in our institution for only 0.2% of surgical ED admissions, interpersonal violence keeps increasing as reflected by the police statistics of our city [24]. In several countries, some trauma units are specifically dedicated to treat specific injuries related to this phenomenon of violence. In Switzerland, the majority of trauma injuries occur in road traffic accidents, as well as during professional and recreational activities. However, as supported by Exadaktylos’s study, it seems that the incidence of violence related injuries is increasing steadily in Switzerland [5]. The majority of patient admitted in our tertiary centre are young males seen during the weekend and at night, presenting with benign injuries that could be treated on an out-patient basis. Few patients needed an emergency operation and only half of these procedures were therapeutic suggesting that a conservative approach should have been considered.
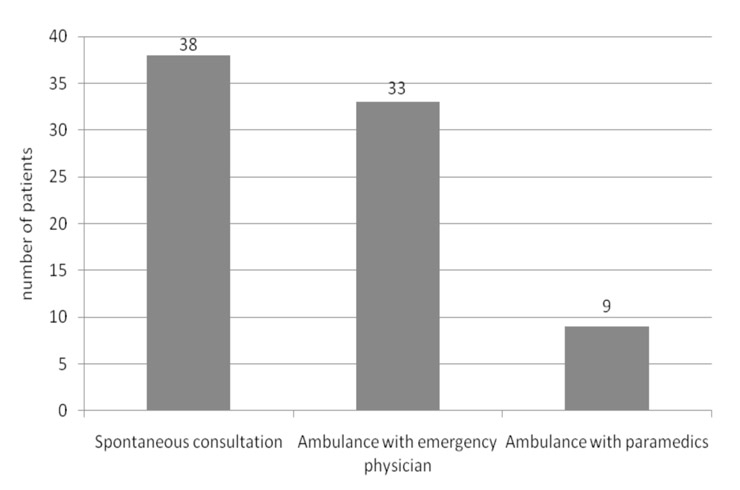
Figure 4
Type of transportation to the ED in our cohort of 80 consecutive stab injuries.
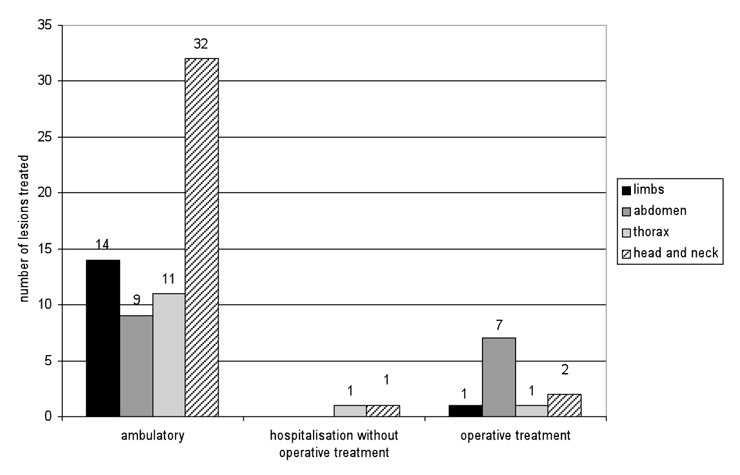
Figure 5
Type of management of the lesions according to their localisation in our cohort of 80 consecutive stab injuries.
Moreover, severe injuries induced by penetrating trauma with the need for operative interventions are even rarer, with only about 5 cases per year (out of 18000 surgical emergency admissions per year). However, due to the absence of a dedicated trauma surgical team in our country, and due to the fact that those penetrating traumas are rare, adequate management of these particular injuries may be nonetheless challenging. It is therefore important to evaluate if our medical structures and surgical skills are adequate to face these types of injuries. The available literature dealing with related-surgical procedures are frequently limited to one anatomic region and thus to a specific surgical specialty [15]. In our series, the pattern of penetrating injuries shows a large majority of superficial wounds, nearly two third of which concerned the upper limbs, the thorax and the abdomen, without involvement of major structures. Injuries involving the full thickness of the thoracic or abdominal wall were rare in our series. This may be possibly due to a locally more developed popular conscience of the potential severity of such trauma.
The main limitation of this study is related to the small number of patients included, especially those with major trauma. The absence of follow up beyond the discharge of the patient also impairs the accurate interpretation of the need for re-hospitalisation and re-operation. Description by the patients of auto-inflicted lesions or non-intentional injuries may in fact represent hidden interpersonal violence and thus underestimate the real prevalence of intentional stab wounds.
Multicentric studies should be undertaken to compare the management of major penetrating trauma in Switzerland to those of high volume level 1 trauma centres in other countries. The inclusion of self-inflicted injuries in such further studies could help to establish local guidelines.
The evidence favouring non-operative treatment of abdominal penetrating trauma is ongoing [19, 20]. Such a therapeutic strategy may be justified in a country with a high incidence of those wounds. Selection of patients eligible for conservative management is based on clinical findings, haemodynamic stability and surgical experience with repetitive accurate clinical assessment based on a standardised algorithm for investigations or imaging. The low incidence of penetrative trauma in our country makes this observational treatment difficult to practice liberally. This could be illustrated in our series by the fact that none of the ten patients operated on for a non-fire arm, penetrating injury were initially selected for a non-operative management while 50% of laparotomies were only diagnostic. This limited experience may also have adverse effects on the timing and other aspects of the decision-making process, especially on the indication for surgery [21–23]. We used laparoscopy as a diagnostic tool to identify lacerations of the parietal peritoneum, regarded as an indication for conversion into a laparotomy. Two laparoscopies were converted into laparotomy, one of which was therapeutic. Even in centres located in higher prevalence areas, the mortality rate of such injuries is usually low, partly due to the fact that penetrating trauma mostly affects young and otherwise healthy patients. The absence of mortality in our series may be explained by the same phenomenon.
Taking into account the low prevalence of penetrating trauma, in our country, even if most of them seem to be benign, a surgical training program in this field should be reconsidered. ATLS® [25] is recognised worldwide as a standard for the management of the trauma patient, but mainly during the first few minutes. Definitive Surgical Trauma Care (DSTC) includes the principles of the ATLS [25] and focuses on the pre and intra operative timing [26]. It helps the surgeon in his decision-making process at each step of patient management from the admission to the ICU. It is dedicated to blunt as well as penetrating trauma. These courses are the baseline of the theoretical teaching. As the prevalence of penetrating trauma is low in Europe, specific surgical skills may be acquired abroad. Creation of exchange programmes may be a part of the answer to the limited experience of surgeons dealing with penetrating trauma. Beyond the scope of the penetrating trauma, these programs would be beneficial to gain skills in the short and mid-term management in all types of trauma. The price to pay to ensure the long term quality of our trauma management may be to finance our trauma surgeons for more stays in foreign level 1 trauma centres. These stays should be integrated into the work plan of the Swiss surgery and EDs.
Stab wound injuries in European countries like Switzerland remain rare. The severity of such injuries is low and observational strategies are considered based on clinical findings and haemodynamic stability.
The authors would like to acknowledge Dr Michael Cotton for proof reading and final translation.
1 Département de Justice et Police, Office Fédéral des migrations. Available on internet: http://www.bfm.admin.ch/bfm/fr/home/themen/statistik/auslaenderstatistik/aktuelle_ergebnisse
2 Exadaktylos A, Stettbacher A, Edul S, et al. Successful management of abdominal stab wounds with clinical evaluation: experiences of a South-African trauma unit with 496 consecutive patients. Unfallchirurg. 2003;106:215–9.
3 CRIPOL (2006). Statistique policière de la criminalité dans le canton de Vaud, année 2006. Available on internet: http://www.police.vd.ch/statistiques/cripol2006/cripol_2006.pdf
4 Meel BL. Incidence and patterns of violent and/or traumatic deaths between 1993 and 1999 in the Transkei region of South Africa. J Trauma. 2004;57:125–9.
5 Exadaktylos A, Häuselmann S, Zimmermann H. Are times getting tougher? A six year survey of urban violence related injuries in a Swiss university hospital. Swiss Med Wkly. 2007;137:525–30.
6 Chiara O, Scott JD, Cimbanassi S, et al. Trauma deaths in an Italian urban area: an audit of pre-hospital and in-hospital trauma care. Injury. 2002;33:553–62.
7 Henderson JP, Morgan SE, Patel F, et al. Patterns of non-firearm homicide. J Clin Forensic Med. 2005;12:128–32.
8 Lyn-Sue J, Siram S, Williams D, et al. Epidemiology of trauma deaths in an urban level-1 trauma center predominantly among African Americans-implications for prevention. J Natl Med Assoc. 2006;98:1940–4.
9 Mac Pherson AK, Schull MJ. Penetrating trauma in Ontario emergency departments: a population-based study CJEM. 2007;9:16–20.
10 Koroukian SM, Beaird H, Duldner JE, et al. Analysis of injury- and violence-related fatalities in the Ohio Medicaid population: identifying opportunities for prevention. J Trauma. 2007;62:989–95.
11 Salim A, Sangthong B, Martin M, et al. Use of computed tomography in anterior abdominal stab wounds: results of a prospective study. Arch Surg. 2006;141:745–52.
12 Inaba K, Munera F, McKenney M, Rivas L, et al. Prospective evaluation of screening multislice helical computed tomographic angiography in the initial evaluation of penetrating neck injuries. J Trauma. 2006;61:144–9.
13 Wong SS. Penetrating Thoracic Injuries: The Use of Transesophageal Echocardiography to Monitor for Complications After Intracardiac Nail Removal. J Trauma. 2008;64:E69–70.
14 Lu KJ, Chien LC, Wo CC, et al. Hemodynamic patterns of blunt and penetrating injuries. J Am Coll Surg. 2006;203:899–907.
15 Van Brussel M, Van Hee R. Abdominal stab wounds: a five-year patient review. Eur J Emerg Med. 2001;8:83–8.
16 Youssef AS, Morgan JM, Padhya T, et al. Penetrating Craniofacial Injury Inflicted by a Knife. J Trauma. 2008;64:1622–4.
17 Doll D, Lenz S, Exadaktylos AK, et al. Penetrating injuries to the pelvis Chirurg 2006;77:770–80.
18 Monneuse OJ, Barth X, Gruner L, et al. Les plaies pénétrantes de l’abdomen, conduite diagnostique et thérapeutique. À propos de 79 patients. Ann Chir. 2004;129:156–6.
19 Demetriades D, Hadjizacharia P, Constantinou C, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244:620–8.
20 Franklin GA, Casós SR. Current advances in the surgical approach to abdominal trauma. Injury. 2006;37:1143–56.
21 Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin North Am. 1997;77:761–77.
22 Rotondo MF, Schwab CW, McGonigal MD, et al. Damage control: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–82.
23 Mattox KL. Introduction, background, and future projections of damage control surgery. Surg Clin North Am. 1997;77:753–9.
24 Lausanne Police statistics: http://www.lausanne.ch/DataDir/LinkedDocsObjDir/10376.pdf
25 Advanced Trauma Life Support for Doctors. American College of Surgeons, Chicago Il. 1997 ed.
26 Boffard KD. Manual of definitive surgical trauma care, London, UK: Hodder/Arnold; 2003.
The authors declare no financial or commercial conflict of interest.