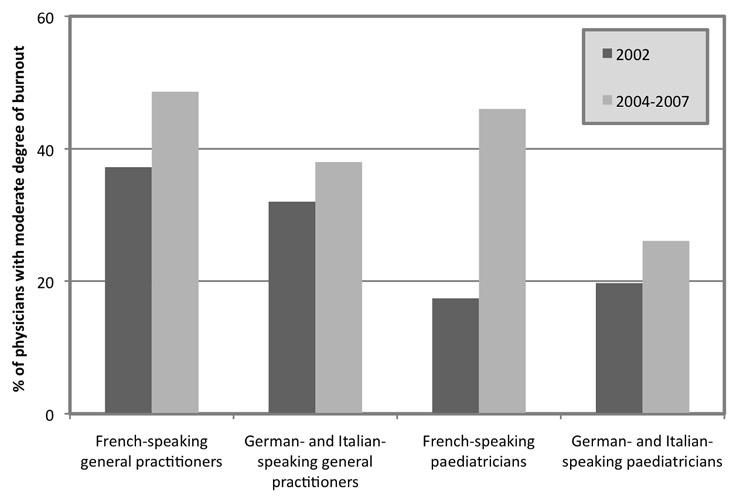
Figure 1
Trends of burnout among Swiss general practitioners and paediatricians.
DOI: https://doi.org/10.4414/smw.2010.13070
In recent years pressure on doctors has risen in many countries as a result of different health care reforms affecting doctors’ autonomy, prestige and income [1–6], resulting in higher work stress. Work stress may result in chronic reactions such as ill health, burnout and depression [7–9]. Burnout occurs when individuals feel emotionally overwhelmed by the demands of their job and may precipitate anxiety and depressive disorders or contribute to self-depreciation [10]. Three dimensions are usually evaluated to detect burnout: 1. emotional exhaustion, reflecting depletion of energy and emotional and cognitive distance from work, 2. depersonalisation or cynicism, involving impersonal thoughts and attitudes towards patients, and 3. a reduced sense of personal accomplishment in one’s work with people or lack of self-efficacy. These three dimensions cannot be combined into a single summary variable. Yet to facilitate analyses and interpretation of scores, some authors have classified doctors with a high level of emotional exhaustion or cynicism as doctors with a moderate degree of burnout [9, 11]. Doctors with a high level of emotional exhaustion and cynicism and a low level of personal accomplishment are generally defined as doctors with a high degree of burnout [12]. There is growing interest in measuring physicians’ health and its determinants, such as burnout [13], because the results of recent research show that physicians’ ill health can negatively affect health care systems and patient care [14–18].
Switzerland is no exception. In recent years several changes have been made in the health care system in an attempt to limit the rise in health care costs. In 1994 a new health insurance law rendered compulsory the purchase by households of a fairly comprehensive package of health benefits, including ambulatory treatment, inpatient care, home nursing care and some health promotion activities. The new law imposed more uniform national standards and sought to achieve greater social solidarity. Basic health insurance cover can be contracted from approximately 90 private insurance carriers, who are precluded from earning profits from the mandated benefit package. Under the new law health care providers are subject to increased competition, a higher administrative burden and decreased work autonomy and income, resulting in higher levels of occupational stress.
A study carried out in 2002 among Swiss primary care practitioners showed that 32% were considered to have a moderate degree and 4% a high degree of burnout [11]. In response to the continuing increase in health care costs, a moratorium was enacted in 2002 to limit accreditation of new community-based providers, including general practitioners. A study conducted in 2004 [19] comparing burnout levels among Swiss cancer clinicians, paediatricians and general practitioners in the French-speaking part of the country found that, overall, one third of the respondents expressed signs indicative of psychiatric morbidity, 44% a moderate degree of burnout (high score on either the dimension of emotional exhaustion or depersonalisation/cynicism) and 6% a high degree of burnout (scores in the range of burnout in all three dimensions). After adjustment for workload, access to continuing education and working in a public institution, French-speaking general practitioners were found to have a higher risk of emotional exhaustion and depersonalisation than cancer clinicians and paediatricians. A similar survey conducted in 2007 in the German- and Italian-speaking parts of the country showed lower prevalences of moderate- and high-degree burnout (32% and 4% respectively, unpublished data), raising the question whether recent health care reforms may have affected the country in different ways or that the situation had improved over time.
In this context we gathered all data from these different surveys and examined the change in burnout prevalence over time across medical specialities and the different language areas of the country.
We compared the data from three cross-sectional surveys conducted in 2002, 2004 and 2007.
The 2002 survey included a country-wide random sample of 2756 certified primary care physicians identified through the membership database of the Swiss Medical Association, including 1098 general practitioners, 986 general internists, 242 paediatricians and 430 physicians without a speciality qualification [11]. Of the 1784 questionnaires returned (answer rate 64.7%), 1755 provided sufficient answers to the Maslach Burnout Inventory (MBI) to classify participants as having a moderate or a high degree of burnout (for additional information, see Survey contentsection below).
The 2004 survey included all cancer clinicians working in the French-speaking part of the country (N = 180) and an equivalent number of general practitioners (N = 197) and paediatricians (N = 184) randomly selected from the registry of their respective medical associations [19]. All physicians had been working for 5 years or more in their speciality and some physicians were still in training. The sub-group of general practitioners and paediatricians was matched for gender according to the oncology sample (40% women). Self-administered questionnaires were sent by mail with up to two reminders. Of the 371 questionnaires returned (answer rate 66.1%), 365 provided sufficient answers to the MBI to classify participants as having a moderate or high degree of burnout.
The 2007 survey included 474 general practitioners, 410 paediatricians and 310 cancer clinicians working in the German- and the Italian-speaking parts of the country. Eligible doctors had been randomly selected from the registry of their respective national medical associations using the same sampling methodology as for the 2004 survey. Of the 620 questionnaires returned (answer rate 51.9%), 615 provided sufficient answers to the MBI to classify participants as having a moderate or high degree of burnout.
The MBI questionnaire has been used to measure the prevalence of burnout [10, 20–22]. The MBI is made up of 22 items on feelings and attitudes towards work which respondents are asked to rate on a 7-point frequency scale. The answers can be summarised as 3 scores reflecting: emotional exhaustion (10 items; e.g. “I feel emotionally drained by my work”); cynicism or depersonalisation (5 items; e.g. “I’ve become more callous towards people since I took this job”), personal accomplishment (7 items; e.g. “I feel I’m positively influencing people’s lives through my work”). Based on a normative sample of 1104 North American medical professionals [12], each respondent can be classified into low, medium and high scores for each dimension. Severe emotional exhaustion is defined as a score ≥27, pronounced cynicism as a score ≥10 and low personal accomplishment as a score ≤33. To facilitate the analysis and interpretation of the scores, we categorized respondents with a high score on either the emotional exhaustion or the cynicism subscales as doctors with a moderate degree of burnout [9, 11]. Respondents with a high score on the emotional exhaustion and cynicism subscales and a low score on the personal accomplishment subscale were defined as doctors with a high degree of burnout [12].
Socio-demographics (gender, living alone, having children) and work-related characteristics (number of years in current workplace, weekly hours worked) were also collected because they are important determinants of burnout and may thus act as confounding factors [10, 23, 24]. The amount of personal information was limited (e.g. age and year of graduation from medical school were not requested) to preserve respondents’ anonymity. As a consequence, the 2007 survey questionnaire included all items in German and Italian, so that respondents’ origin could not be differentiated between these two regions.
Descriptive statistics, including cross-tabulation, χ2 test and analysis of variance, were used to compare the socio-demographic and work-related characteristics of the respondents across the different surveys. Prevalences of moderate- and high-degree burnout were stratified by medical specialities and linguistic areas of the country for each survey. Fisher’s exact test and χ2 test were used to test differences between subgroups where appropriate. To study the relationships of socio-demographic and work-related characteristics with burnout, cross-tabulation and χ2 test were used to identify potential confounders. Finally, logistic regression models were used to identify multivariate predictors of moderate and high degree of burnout, with region (French-speaking vs. Italian- and German-speaking), medical speciality (general practitioners, including general internists vs. all others), time of survey (2002 vs. 2004 & 2007) and significant socio-demographic and work-related characteristics as predictors. As the 2004 and 2007 survey had not been conducted in all linguistic areas, they were grouped together and compared to data collected in 2002. To investigate whether the risk increased differentially over time, interaction terms between significant factors were used whenever the factor “time of survey” was significant. All statistical tests were two-tailed, with a significance level of 0.05.
The majority of participants were men, had children and were living with a partner (table 1). Differences in gender and medical speciality distributions across the surveys were significant, reflecting the different sampling procedures. The number of years in the current workplace was lower for the 2004 and 2007 surveys because these samples also included physicians in training not yet working as community-based physicians. No difference was found for self-reported work time per week.
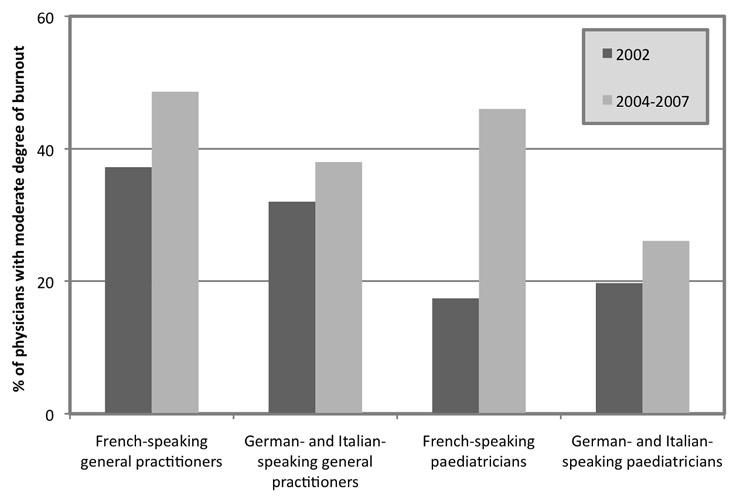
Figure 1
Trends of burnout among Swiss general practitioners and paediatricians.
General practitioners reported the highest prevalence of moderate-degree burnout in 2002 and 2007 (table 2). The increase over time was significant for French-speaking general practitioners and paediatricians. Rates of moderate degree of burnout increased from 33% to 42% among general practitioners (p = 0.002) and from 19% to 34% among paediatricians (p = 0.001). No significant difference over time was found for general practitioners and paediatricians presenting a high degree of burnout (4% to 6% [p = 0.17] and 2% to 4% [p = 0.42] respectively).
Besides the effects of time, medical speciality, linguistic region of the survey, male gender and working over 50 hours per week were associated with higher levels of burnout (table 3).
After adjustment for gender and total work time per week, an increased risk of moderate burnout was found for physicians surveyed in 2004 and 2007 (OR 1.6, 95%CI 1.3 to 2.0), general practitioners (OR 1.6, 95%CI 1.3 to 2.0) and physicians living in the French-speaking region of the country (OR 1.5, 95%CI 1.3 to 1.9) (table 4). An increased risk of high degree of burnout was found only for general practitioners (OR 1.8, 95%CI 1.05 to 3.0). The interaction term between time of the survey (2002 vs. 2004 & 2007) and linguistic region was also significant, indicating an additional risk over time for doctors in the French-speaking part of the country.
On the basis of the unadjusted results (fig. 1), we also tested whether paediatricians were at increased risk over time by including a dummy variable for paediatricians in the regression models. After adjustment for all other factors, paediatricians were not found to be at increased risk of burnout.
| Table 1Socio-demographic characteristics of 2735 Swiss doctors surveyed by the Maslach Burnout Inventory between 2002 and 2007. | ||||
| 2002 | 2004 | 2007 | ||
| (N = 1755) | (N = 365) | (N = 615) | p-value 2 | |
| Women, N (%)1 | 282 (16.1) | 126 (34.8) | 202 (33.4) | <0.001 |
| Living alone, N (%) | 195 (11.1) | 62 (17.0) | 170 (27.6) | <0.001 |
| Having children, N (%) | 1177 (67.1) | 281 (77.0) | 419 (68.1) | 0.001 |
| Region, N (%) | <0.001 | |||
| German- and Italian-speaking | 1329 (75.7) | – | 615 (100) | |
| French-speaking | 426 (24.3) | 365 (100) | – | |
| Medical speciality, N (%) | <0.001 | |||
| General practitioners | 838 (47.7) | 140 (38.4) | 266 (43.3) | |
| Paediatricians | 163 (9.3) | 113 (31.0) | 188 (30.6) | |
| General internists | 440 (25.1) | – | – | |
| Cancer clinicians | – | 112 (30.7) | 161 (26.2) | |
| Internal medicine specialists | 149 (8.5) | – | – | |
| No FMH | 165 (9.4) | |||
| Number of years in current workplace, mean (SD) | 15.2 (8.2) | 11.1 (8.7) | 10.5 (7.8) | <0.0013 |
| Estimated total work time (hours), mean (SD) | 51.2 (14.4) | 50.5 (14.2) | 51.4 (15.3) | 0.643 |
| 1 Information on gender was missing for 19 respondents2 χ2 test3 ANOVA, comparison of the means | ||||
| Table 2Distribution of burnout among 2735 Swiss general practitioners, paediatricians, internal medicine specialists and cancer clinicians across different regions of the country in 2002, 2004 and 2007. | ||||||||
| Physicians with moderate degree of burnout | Physicians with high degree of burnout | |||||||
| 2002 | 2004 | 2007 | 2002 | 2004 | 2007 | |||
| % (n/N) | % (n/N) | % (n/N) | p-value1 | % (n/N) | % (n/N) | % (n/N) | p-value1 | |
| Overall | 31.5 (553/1755) | 44.4 (162/365) | 31.5 (194/615) | <0.001 | 3.5 (62/1755) | 6.3 (23/365) | 3.7 (23/615) | 0.045 |
| General practitioners | ||||||||
| French-speaking | 37.2 (125/336) | 48.6 (68/140) | – | 0.02 | 2.7 (9/336) | 5.7 (8/140) | – | 0.11 |
| German- and Italian-speaking | 32.0 (354/1107) | – | 38.0 (101/266) | 0.07 | 4.3 (48/1107) | – | 5.6 (15/266) | 0.41 |
| Paediatricians | ||||||||
| French-speaking | 17.4 (8/46) | 46.0 (52/113) | – | 0.001 | 2.2 (1/46) | 7.1 (8/113) | – | 0.45 |
| German- and Italian-speaking | 19.7 (23/117) | – | 26.1 (49/188) | 0.22 | 1.7 (2/117) | – | 1.6 (3/188) | 1.0 |
| Internal medicine specialists | ||||||||
| French-speaking | 29.5 (13/44) | – | – | NA | 0.0 (0/44) | – | – | NA |
| German- and Italian-speaking | 28.6 (30/105) | – | – | NA | 1.9 (2/105) | – | – | NA |
| Cancer clinicians | ||||||||
| French-speaking | – | 37.5 (42/112) | NA | – | 6.2 (7/112) | – | NA | |
| German- and Italian-speaking | – | 27.3 (44/161) | NA | – | – | 3.1 (5/161) | NA | |
| p-value2 | 0.001 | 0.20 | 0.01 | 0.12 | 0.91 | 0.07 | ||
| 1 Fisher’s exact test, comparison between surveys for each region; NA: not available.2 χ2 test, comparison between medical specialities for each survey. | ||||||||
| Table 3Relationships between socio-demographic characteristics and burnout among 2735 Swiss general practitioners, paediatricians, internal medicine specialists and cancer clinicians. | |||||
| Physicians with moderate degree of burnout | Physicians with high degree of burnout | ||||
| N | % | p-value | % | p.value | |
| Gender (19 missing) | <0.001 | 0.008 | |||
| Male | 2106 | 35.4 | 4.5 | ||
| Female | 610 | 26.1 | 2.1 | ||
| Living in couple | 0.12 | 0.26 | |||
| Yes | 2308 | 32.6 | 3.8 | ||
| No | 427 | 36.5 | 4.9 | ||
| Has children | 0.37 | 0.38 | |||
| Yes | 1877 | 33.8 | 3.7 | ||
| No | 858 | 32.1 | 4.4 | ||
| Nb of years in current workplace(95 missing) | 0.13 | <0.24 | |||
| 1–5 | 575 | 32.5 | 4.2 | ||
| 6–10 | 507 | 33.3 | 2.6 | ||
| 11–15 | 474 | 38.0 | 5.1 | ||
| >15 | 1086 | 32.0 | 4.1 | ||
| Estimated total work time(hours per week)(81 missing) | <0.001 | <0.001 | |||
| <45 | 699 | 24.5 | 1.6 | ||
| 45–53 | 751 | 35.6 | 3.7 | ||
| 54–60 | 644 | 37.4 | 6.1 | ||
| >60 | 560 | 36.2 | 4.1 | ||
| 1 χ2 test | |||||
| Table 4Mutlivariate predictors of burnout among 2735 Swiss physicians. | ||||
| Moderate degree of burnout | High degree of burnout | |||
| OR 1 | CI 95% 1 | OR 1 | CI 95% 1 | |
| Time of survey | ||||
| 2004 & 2007 survey (vs. 2002 survey) | 1.6 | 1.3 to 2.0 | 1.4 | 0.9 to 2.3 |
| Gender | ||||
| Men (vs. women) | 1.4 | 1.1 to 1.8 | 1.5 | 0.8 to 3.0 |
| Number of years in current workplace(vs. >15 years) | ||||
| 1–5 years | 1.1 | 0.9 to 1.5 | 1.3 | 0.7 to 2.2 |
| 6–10 years | 1.3 | 1.0 to 1.6 | 0.7 | 0.4 to 1.4 |
| 11–15 years | 1.4 | 1.1 to 1.7 | 1.3 | 0.8 to 2.2 |
| Estimated total work time (vs. <45 hours) | ||||
| 45–53 hours | 1.6 | 1.2 to 2.0 | 2.0 | 1.0 to 4.2 |
| 54–60 hours | 1.7 | 1.3 to 2.2 | 3.3 | 1.6 to 6.7 |
| >60 hours | 1.7 | 1.3 to 2.2 | 2.3 | 1.1 to 5.0 |
| Region | ||||
| French-speaking (vs. German- and Italian-speaking physicians) | 1.5 | 1.3 to 1.9 | 1.0 | 0.6 to 1.6 |
| Medical speciality | ||||
| General practitioners (vs. paediatricians & other specialists) | 1.6 | 1.3 to 2.0 | 1.8 | 1.05 to 3.0 |
| Interaction term | ||||
| French-speaking x 2004–2007 survey | 1.5 | 1.01 to 2.1 | - | - |
| 1 Odds ratio and 95% CI are adjusted for all other factors listed in the table. | ||||
Burnout levels among Swiss doctors have increased throughout the country over the last decade. The risk of moderate burnout was higher for general practitioners and French-speaking doctors. Also, the increase was significantly higher for French-speaking doctors over time.
Amongst the few authors who have investigated burnout levels longitudinally, Taylor et al. [25] observed a decline in the mental health of UK physicians varying according to the medical speciality. In this study the proportion of clinical oncologists showing excessive emotional exhaustion increased from 39% to 52% over 8 years. This trend was interpreted as related to a workload increase following reconfiguration of cancer services, concomitant with a decrease in job satisfaction.
In the literature general practitioners have been previously considered to be at increased risk of experiencing stress-related suffering when compared to other medical specialists [26, 27]. Compared to other industrialised countries, Swiss primary care physicians were apparently less affected by burnout in 2002 [11]. Goehring et al. [11] have found that risk factors of moderate burnout for Swiss primary care practitioners were male gender, age between 45–55 years, higher levels of perceived stress related to the health insurance workload, changes in the health care system, medical care uncertainty, and increased difficulties in balancing professional and private life.
As in other countries, many reforms have been undertaken in recent years in an endeavour to control health care costs. The use of the new uniform national relative value scale and the aging of practising primary care physicians following the moratorium probably resulted in differential worsening of working conditions for general practitioners throughout the country [28]. Our results suggest that these changes bore more heavily on French-speaking doctors.
Results of recent work by Buddeberg-Fischer et al. [29, 30] on a cohort of young Swiss German-speaking doctors in training are also worrying. They have found that only a minority (from 10–16%) plan to practice general medicine due to the uncertain development of health policy, decreasing income and worsening working conditions.
To balance the effects of increased pressure at work and work-related stress, common strategies at an individual level include valuing relationships with patients [5], participating in continuing medical education [5, 31], and participation in Balint groups [32]. However, at the health-care system level, only initiatives that have addressed the issues of appropriate remuneration and workload have been able to reverse the current trend of degrading working conditions for general practitioners. The introduction of the new general medical services (GMS) contract in the UK resulted in a sharp increase in general practitioners’ satisfaction [33]. Among other ways of making general practice more attractive, promotion of group practice is also important. Indeed, in a recent survey 88% of young Swiss general practitioners were planning to work in group practice [28].
In this paper we used data from three different large surveys based on the same validated instruments allowing comparison with other published studies. The analysis of these data [11, 19] over the years provides some important information about the trend in physicians’ morale in an era of major health care reforms in Switzerland.
The study also suffers from several limitations. The response rate varied significantly between 2004 and 2007 (66% vs. 52%). This could be partly due to the fact that the questionnaire used in 2007 included both German and Italian items and was therefore much longer, a factor that can lower the response rate. Participants may also have suffered more frequently from burnout that non-participants, thus overestimating the true rate in our samples. In a previous study we found that participants in the survey were more likely to report burnout, but that this difference was weak [11]. Further, differences in respondents’ characteristics across the surveys may have acted as confounding factors. To allow for this possibility we used several regression models to identify significant risk factors and interaction terms.
We have found an increasing prevalence of burnout among Swiss doctors over time, especially in the French-speaking part of the country. This result may be the sign of a differential effect of current health care reforms and policies or of practice style throughout the country. Protective factors against the risk of burnout, such as participation in continuing education or large group practice, [28, 31] may differ between linguistic regions. Among adverse factors, despite the new uniform national relative value scale, there is an increasing asymmetry in income among physicians across the country [34, 35]. In most cantons of the German-speaking part of Switzerland, general practitioners are allowed to sell the drugs they prescribe to their patients and make a profit on this sale, which generates a significant amount of their revenue. In a recent published paper we showed that satisfaction with current income can “buffer” the effect of emotional exhaustion on physicians’ mental health [36]. We hypothesise that the difference in burnout prevalence between French- and German-speaking physicians may be related to this income difference, especially for primary care practitioners. As Swiss public health authorities are now discussing ending the sale of drugs by primary care practitioners, representative surveys should be conducted regularly to document the impact of such changes on Swiss doctors’ levels of wellbeing and ill health in coming years, using a standardised methodology to minimise the risk of measurement bias and confounding.
We would like to thank all the physicians who took the time to participate and respond to the surveys, Mesd. Paola Pirelli, Chantal Gazzola-Manfrini, Florence Marti Klay and Delphine Squiban for their administrative work and Dr Jill Graham for her methodological advice.
1 Sibbald B, Enzer I, Cooper C, Rout U, Sutherland V. GP job satisfaction in 1987, 1990 and 1998: lessons for the future? Fam Pract. 2000;17:364–71.
2 Sibbald B, Bojke C, Gravelle H. National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ. 2003;326:22.
3 MacKean P, Gutkin C. Fewer medical students selecting family medicine. Can family practice survive? Can Fam Physician. 2003;49:408–9, 15–7.
4 Thommasen HV, Lavanchy M, Connelly I, Berkowitz J, Grzybowski S. Mental health, job satisfaction, and intention to relocate. Opinions of physicians in rural British Columbia. Can Fam Physician. 2001;47:737–44.
5 Lee FJ, Stewart M, Brown JB. Stress, burnout, and strategies for reducing them: what›s the situation among Canadian family physicians? Can Fam Physician. 2008;54:234–5.
6 Bodenheimer T. Primary care – will it survive? N Engl J Med. 2006;355:861–4.
7 McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359:2089–90.
8 Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724–8.
9 Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–67.
10 Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422.
11 Goehring C, Bouvier Gallacchi M, Kunzi B, Bovier P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med Wkly. 2005;135:101–8.
12 Maslach C, Jackson S, Leiter MP. Maslach Burnout Inventory Manual. Third edition, Palo Alto, CA: Consulting Psychologist’s Press, 1996.
13 Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–21.
14 Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–91.
15 Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–22.
16 Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 351:1829–37.
17 Shanafelt TD, West C, Zhao X, Novotny P, Kolars J, Habermann T, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559–64.
18 West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–8.
19 Arigoni F, Bovier PA, Mermillod B, Waltz P, Sappino AP. Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: who are most at risk? Support Care Cancer. 2009;17:75–81.
20 Dion G, Tessier R. Validation de la traduction de l’inventaire d’épuisement professionnel de Maslach et Jackson. Revue canadienne des sciences du comportement 1994;26:210–27.
21 Bussing A, Perrar KM. Burnout measurement. Study of a German version of the Maslach Burnout Inventory (MBI-D). Pflege Z. 1994;47(suppl):20–30.
22 Sirigatti S, Stefanile C. Adattamento italiano MBI – Maslach Burnout Inventory, Firenze: Organizzazioni Speciali, 1993.
23 Graham J, Potts HW, Ramirez AJ. Stress and burnout in doctors. Lancet. 2002;360:1975–6; author reply 76.
24 Schaufeli WB, Enzmann D. The burnout companion to study and practice: a critical analysis. Issues in occupational health, London: Taylor & Francis, 1998.
25 Taylor C, Graham J, Potts HW, Richards MA, Ramirez AJ. Changes in mental health of UK hospital consultants since the mid-1990s. Lancet. 2005;366:742–4.
26 Kushnir T, Cohen AH. Job structure and burnout among primary care pediatricians. Work. 2006;27:67–74.
27 Virtanen P, Oksanen T, Kivimaki M, Virtanen M, Pentti J, Vahtera J. Work stress and health in primary health care physicians and hospital physicians. Occup Environ Med. 2008;65:364–6.
28 Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. The new generation of family physicians – career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138:305–12.
29 Buddeberg-Fischer B, Dietz C, Klaghofer R, Buddeberg C. Swiss residents’ arguments for and against a career in medicine. BMC Health Serv Res. 2006;6:98.
30 Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C. Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health. 2008;82:31–8.
31 Brondt A, Sokolowski I, Olesen F, Vedsted P. Continuing medical education and burnout among Danish GPs. Br J Gen Pract. 2008;58:15–9.
32 Kjeldmand D, Holmstrom I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med. 2008;6:138–45.
33 Whalley D, Gravelle H, Sibbald B. Effect of the new contract on GPs’ working lives and perceptions of quality of care: a longitudinal survey. Br J Gen Pract. 2008;58:8–14.
34 de Haller J. Le revenu des médecins. Bulletin des médecins suisse 2009;90:407.
35 Reichert M. Revenu des médecins indépendants de Suisse en 2006 (nouveau) et 2005 (réévaluation). Bulletin des médecins suisse 2010;91:479–87.
36 Bovier PA, Arigoni F, Schneider M, Gallacchi MB. Relationships between work satisfaction, emotional exhaustion and mental health among Swiss primary care physicians. Eur J Public Health. 2009;19:611–7.
This research project was partly supported by research grants from the institutional funds of the Division of Oncology and the Department of General Internal Medicine of the Geneva University Hospitals and from Amgen, Switzerland.