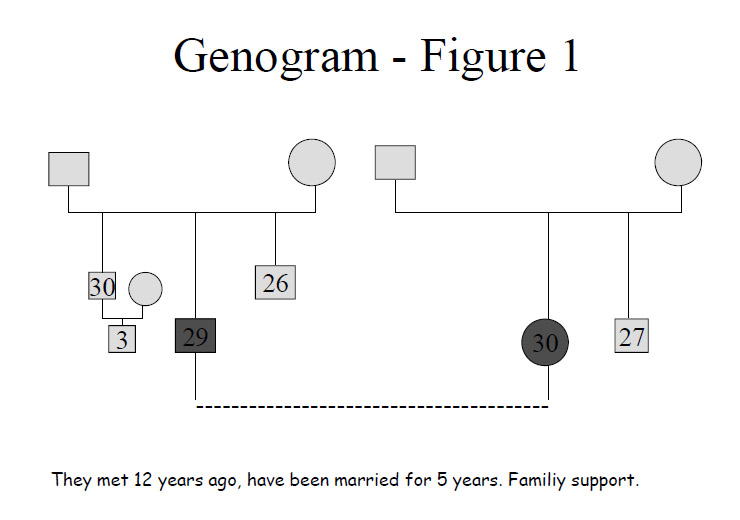
Figure 1
Counselling of the two partners. Very stable relationship. The couple is shocked by the diagnosis of cancer but is very well supported (family and external support). They decide to freeze pronucleids.
DOI: https://doi.org/10.4414/smw.2010.13075
Psychological support in young women who contemplate emergency assisted reproductive technologies (ART) prior to chemo- and/or radiation-therapy
Women of reproductive age who are diagnosed with cancer (breast cancer, lymphomas or other types of cancer) express a need to discuss the bearing their disease and treatment may have on their future fertility. The chemo- and/or radiotherapy undertaken to treat their cancer may indeed transitorily or definitively hamper ovarian function, leading to amenorrhoea and/or infertility. The gravity of these consequences and their duration – and hence, the grounds for implementing fertility protection measures – greatly depend on the type of cancer and treatment received, as well as the age and specific susceptibilities of each patient.
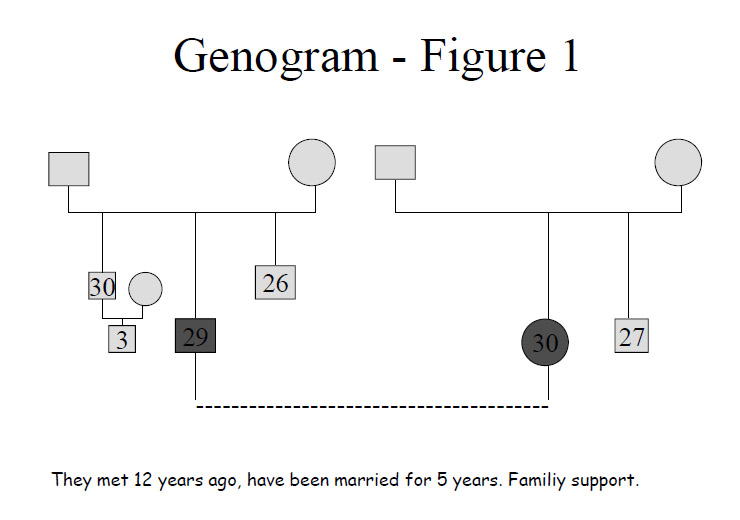
Figure 1
Counselling of the two partners. Very stable relationship. The couple is shocked by the diagnosis of cancer but is very well supported (family and external support). They decide to freeze pronucleids.
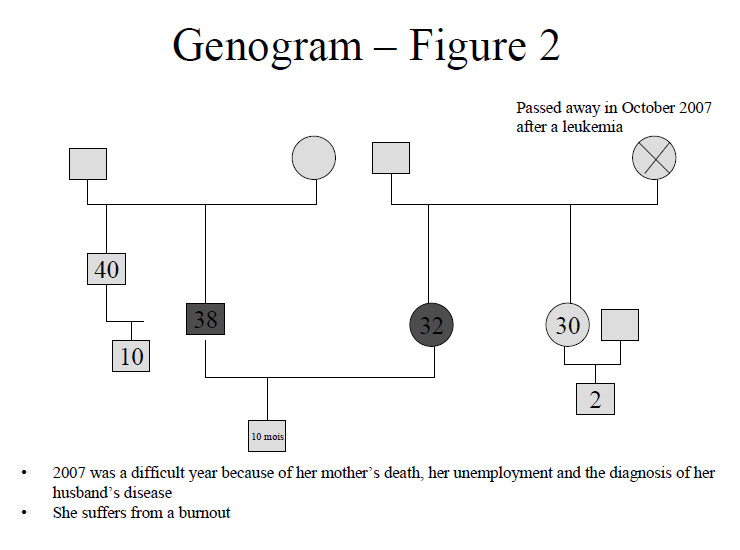
Figure 2
Counselling of the two partners. The couple had already begun a couple therapy before the diagnosis. They have to ask the family to pay for the treatment. The couple prefers freezing oocytes and pronucleids.
In an effort to optimise the counselling on possible measures to preserve fertility we created a multidisciplinary cancer and fertility task force within the linguistically-defined area of French-speaking Switzerland. This structure, identified as the “Réseau Romand de Cancer et Fertilité”, groups together practitioners in oncology, oncogynaecology, surgery, paediatrics, psychiatry and gynaecology specialised in reproductive medicine. The aims set for the task force were to counsel for, establish and coordinate possible fertility-preserving measures tailored to the cancer problem, personal characteristics and treatment envisaged [1]. Furthermore, the task force was convened on clearly formulated consensual guidelines and specific recommendations best meeting fertility preserving concerns and cancer imperatives for the different types of cancer. These were published in the form of articles and booklets targeted at the medical practitioners of French-speaking Switzerland [1–3] and are accessible online [2]. While not exactly reproducing other existing guidelines, the Task Force booklets are in general agreement with the recommendations of other societies.
In close collaboration with the attending physicians, specific psychological counselling is offered to each patient or couple concerning the possible options for fertility preservation and their implications in cancer patients. The literature abounds in recommendations favouring the offer of counselling, yet the published articles provide limited information on the type of approach that is best suited to the needs of cancer patients concerned about their fecundity. Strategies are the communication skills of active listening typically used in a patient-centred approach [4, 5]. In practice our approach constitutes an extension of the techniques of preventive counselling routinely offered to all infertile couples undergoing ART at our institution (Women`s Hospital, CHUV, Lausanne) [6, 7]. This assistance has been developed and conceptualised over the last 18 years as part of the collaboration between clinical practitioners in medically assisted procreation, sexual and reproductive health counsellors, psychologists and psychiatrists [6, 7]. The primary advantage of this counselling approach is its rapid effectiveness in sorting out possible difficulties. Cancer patients are forced to make instant decisions because of the urgency of cancer treatment. The counselling is used in these cases to assess rapidly the woman’s (couple’s) resources in order to choose the best option for each woman’s specific situation. The so-called genogram is used as a select tool in resources evaluation [8]. It involves joining with the couple in building a genealogical tree during the interview by representing their families of origin (but also their relatives and friends if they have a significant relationship with the couple). Notes or lines are added to show the relationships between the individuals. By building the genogram together the necessary investigations are given a natural and coherent direction and the biographical issues and the couple’s interactions can be highlighted. Figures 1, 2, 3 and 4 outline this technique.
The aim is to offer psychological support to each couple during the treatment. At the first counselling session the couple’s emotional state is evaluated and their relationship with the nursing staff fostered. It also serves to assess the couple’s capacity to cope with the unforeseeable events during/after the treatment (stress, possible failure, transition to parenthood) in order to define the most adequate type of psychological assistance.
Counselling of cancer patients occurs in a special context: the shock after the diagnosis of cancer and the urgency of treatment, the fragility of life with the idea of possible death (despite the outstanding cure rates of many cancers, cancer still frightens), to which is added the issue of possible future infertility and its prevention, all of which was not necessarily on the agenda. The woman (couple) is not prepared for that possibility but must face up to it: hence it is in these particular circumstances that the counselling may best help.
The sources of stress that arise from cancer and fertility issues are multiple. First, the emergency ART that may be envisaged does not guarantee pregnancy after cancer. Nor is the patient even certain of ever using the preserved gametes or pronucleids (PNs) – in spite of the cost borne in countries such as Switzerland where ART is self-financed – because recovery of spontaneous fecundity is not that uncommon. This is particularly the case in breast cancer, the most common situation where emergency ART is contemplated [9]. Success of emergency ART depends on numerous factors related or not to the disease itself: the number of oocytes harvested will vary according to the patient’s chronological and biological age (ovarian reserve) and general health. Currently, success rates are higher when PNs rather than unfertilised oocytes are cryopreserved.
The aim of our study was to gain insight into the different situations. Specifically, we tried to identify the typical patterns encountered in women and couples that prompt them to either seek or renounce fertility preservation measures.
The primary objective of counselling was to provide information and ease the decision-making process while providing support. The ultimate goal is therefore to provide information, discuss the possible options and support the decision that is ultimately taken.
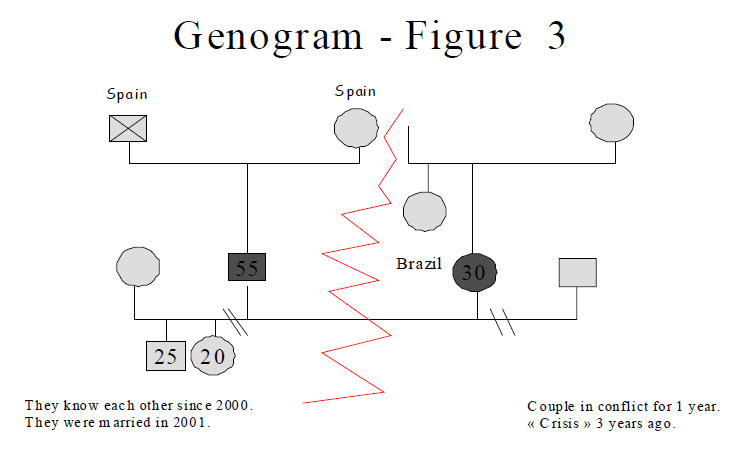
Figure 3
Counselling of the two partners. The couple was in conflict before the disease. They decide to freeze unfertilised oocytes. Couple therapy was suggested.
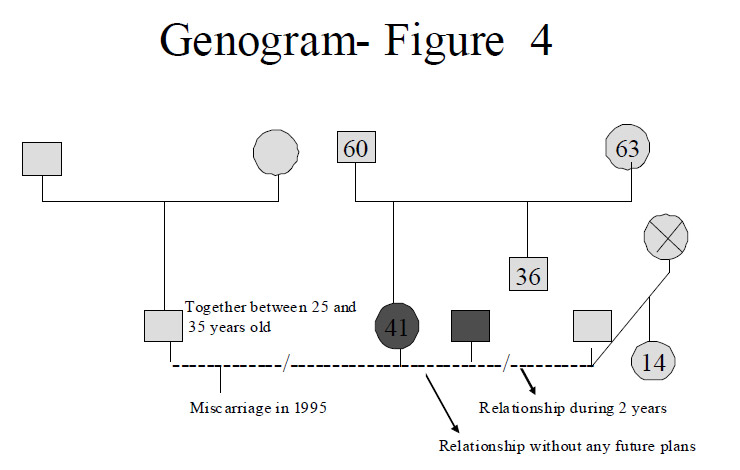
Figure 4
Patient seen alone. Patient in a couple without future plans. Patient wants to take care of herself and of her health first. Declines the ART programme. Thinks she can resort to oocyte donation later abroad (not allowed in Switzerland according to the law on medically assisted procreation LPMA [7]).
Information is given on:
1. The treatment options: the option to freeze either unfertilised oocytes, if the woman has no partner, or PNs, if the couple already has a clearly established desire to found a family. In certain cases split option may be preferred, with both oocytes and PNs being cryopreserved if the size of the harvest permits. Swiss law on medically assisted procreation (LPMA) stipulates that “medically assisted procreation is subordinated to the well-being of the child” (LPMA, Art. 3) [10], implying therefore a stability of the couple undergoing ART.
2. Treatment costs (CHF 6000–8000) are not covered by the Swiss health insurance, as ART in general is not covered. The couple will also need to pay for the embryo transfer (CHF 1500–2000/transfer) when this takes place after the cancer treatment. Also, certain centres charge yearly fees for keeping cryopreserved PNs or gametes, although these are usually limited in amount (CHF 200–300/year).
3. Unforeseeable complications of the treatment and the fact that ART’s successful completion cannot be guaranteed (insufficient ovarian responses, cancellations and other mishaps being possible).
4. The fertility treatment should not alter the chances of cancer treatment by, for example, unduly delaying the beginning of chemotherapy. This important point must be clarified by the oncologist with each patient. Essential to this is the need to address fertility issues early in the process, not on the eve of the scheduled chemotherapy when there is no time left for possible measures.
5. The time interval before pregnancy can be contemplated and the fact that it is dependent upon full recovery from cancer also needs to be discussed. Full agreement of the oncologist to any envisaged measure and confirmation of the patient’s reasonable chances of recovery must also be obtained. This is in particular necessary in order to comply with Swiss ethical law stipulating that ART is for individuals “who are able to bring up the child until his/her majority” (LPMA, Art. 3, b) [10].
6. The duration of cryopreservation of unfertilised oocytes is normally limited to 5 years, but can be legally extended in the case of cancer under Swiss law (LPMA, Art. 15) [10]. The duration of cryopreservation of PNs is theoretically limited to 5 years by Swiss Law, although provisions similar to those enacted for gametes [10] are currently under discussion.
Building the genogram [8] in conjunction with the couple, as explained above, enables us to rapidly highlight the important features of their individual and common life story and eases the discussion on the advisability of the various options:
1. The couple is more or less stable; having a child has already been discussed or even attempted. In this case, the couple would rather freeze PNs. This situation is illustrated in fig. 1 where the couple already had built their house in anticipation of founding a family.
2. The couple is stable, but the issue of childbearing only became acute because of the urgency created by cancer. The couple may in this case go for a split option, freezing both PNs and oocytes provided that the oocyte harvest is sufficient. This compromise option preserves some fertility potential in the event that the couple break up. This is illustrated in fig. 2, where the couple had encountered issues of disagreement already serious enough to warrant therapy before cancer was diagnosed in the female partner. Although they already had a child, they were not decided about the prospect of having another one together.
3. The woman is single or the current couple has no desire for children. The woman wishes to remain able to procreate later. In this case she will choose oocyte freezing. Fig. 3 illustrates a situation where the presence of an existing conflict in the couple led to this choice.
4. The woman (couple) has no desire for a child. The urgency is for the cancer treatment. In this case, emergency ART would only generate further stress and is not desired. In this case the woman (couple) declines the fertility preservation options. She is likely to express gratitude for the fact that the issue was brought up and thoroughly discussed with her, thus helping her to clarify her personal position. Fig. 4 shows the situation in which a woman was not in a significant relationship when her cancer was diagnosed and she declined the ART programme.
5. The woman (couple) does not have the needful financial resources to contemplate ART, which they must thus decline. This situation is experienced as particularly unfair.
Assisting the woman and/or the couple is achieved through a person-based listening. It is crucial to know the characteristics of the particular cancer, its typical course and prognosis and the type of treatment needed. It is likewise important to survey the psychological, socioeconomic and family dimensions forming the context of any given cancer and fertility issue encountered. The disease is a cause of stress, as it drastically changes life plans and especially the questions pertinent to childbearing. All the person’s and couple’s own resources need to be mustered in order to face this unexpected – and deemed unfair – stroke of fate. The quality of the couple’s relationship (if there is a couple), the support given by the family circle, family, friends and colleagues become important, as well as the individual capacity to face problems. The counsellor remains at the woman’s or couple’s disposal and is ready to see her/them again as needed. At times when it appears necessary and/or desirable the counsellor can also guide either the woman or the couple towards long-term support (psychiatrist, psychologist, couple counselling or other types of support).
From January 2007 to September 2009, 23 patients/couples went through the special cancer and fecundity personal resources counselling offered at UMR-CHUV in the context of the dedicated task force “Réseau Romand de Fécondité et Cancer”. Individual details of this population are given in table 1. In this table only patients/couples who have undergone psychological counselling before therapy are listed. The primary purpose was to offer women diagnosed with cancer the option of, and necessary guidance in, properly thinking through the bearing of their cancer and its treatment on their further fecundity and contemplating the fertility preserving options possible. The time frame for enacting such fertility measures such as, for example, emergency ART is often restricted, being of a few weeks at the maximum. It is also a privileged opportunity to plan ahead for life after cancer and help shape a positive and optimistic yet realistic vision.
Of 23 counselling sessions provided to date, 18 were to couples and 5 to single women. The mean age of the women undergoing fertility preservation methods was 32.3 years. Twenty of these couples/women elected to act on fertility preserving options (one patient was excluded due to biological age). Conversely, only 2 single women elected not to initiate any fertility preserving measure. In total, 19 emergency ART cycles were initiated. In 8 cases (42%), PNs were frozen, in 7 (37%) oocytes (with one case of empty follicle syndrome), and a mix of oocytes and PNs in the remaining 4 (21%). In one case the only alternative for fertility preservation was ovarian tissue cryopreservation.
| Table 1Patients who were offered psychological counselling within the framework of the programme “Cancer and Fertility” at the University Women’s Hospital, CHUV, Lausanne. | ||||||
| Nbr | Diagnosis | Age | Marital status | Children | Results of fertility preservation | |
| 2007 | 1 | Breast cancer | 38 | Couple (m.) | 2 | 2 oocytes |
| 2 | Hodgkin’s lymphoma | 27 | Couple (n. m.) | None | 6 oocytes, 12 PNs | |
| 3 | Breast cancer | 25 | Couple (n. m.) | None | 3 PNs | |
| 4 | Breast cancer | 36 | Couple (n. m.) | 1 | 8 PNs | |
| 5 | Breast cancer | 37 | Single | None | Declines ART | |
| 6 | Breast cancer | 29 | Couple (n. m.) | None | 1 PNs | |
| 7 | Breast cancer | 39 | Single | None | Declines ART for psychological reasons | |
| 2008 | 8 | Breast cancer | 34 | Couple (m.) | None | 20 oocytes, couple in conflict |
| 9 | Breast cancer | 34 | Couple (m.) | 1 | 9 oocytes | |
| 10 | Breast cancer | 32 | Couple (m.) | None | 6 oocytes, 7 PNs | |
| 11 | Hodgkin’s lymphoma | 21 | Single | None | 15 oocytes | |
| 12 | Breast cancer | 28 | Couple (n. m.) | None | 4 PNs | |
| 13 | Inflammatory disease (chemotherapy) | 27 | Couple (m.) | None | 2 PNs | |
| 14 | Breast cancer | 33 | Couple (n. m.) | None | 6 PNs | |
| 15 | Breast cancer | 39 | Couple (n. m.) | None | No oocyte in spite of hormonal stimulation of the ovary (empty follicle syndrome) | |
| 16 | Breast cancer | 28 | Couple (m.) | 1 | 9 PNs | |
| 2009 | 17 | Breast cancer | 34 | Couple (n. m.) | None | Has to decline to freeze oocytes because she starts chemotherapy at once. Has frozen ovarian tissue. |
| 18 | Breast cancer | 31 | Couple (m.) | None | 11 oocytes, 8 PNs | |
| 19 | Breast cancer | 25 | Single | None | 17 oocytes | |
| 20 | Breast cancer | 43 | Divorced, new couple (n. m.) | 1 | Has to decline because of age | |
| 21 | Breast cancer | 37 | Couple (m.) | 1 | 1 PN | |
| 22 | Breast cancer | 38 | Single | None | 5 oocytes | |
| 23 | Breast cancer | 39 | Couple (n.m.) | None | 6 oocytes, 6 PNs | |
| m. = marriedn.m.= not marriedPN(s) = pronucleid(s) | ||||||
Our long experience of routinely counselling all-comer infertile couples gave us the background and tools to develop special counselling on cancer and fecundity issues. Despite the emergency and stressful characteristics of the situation, we believe it is of the utmost importance to take the necessary time to inform patients about the reproductive implications of their cancer and its treatment. We believe that the tools developed at our institution as an offshoot of the “personal resource assessment” routinely offered to infertility patients undergoing ART is a practical means of optimising the reproductive counselling and support offered to cancer patients. One important feature of our approach is that it is time-restricted and thus effective at assisting couples in what most often amounts to an emergency situation.
To comfort the patient (couple) in her (their) decision it is necessary to discuss the matter thoroughly with the patient (couple), to take into account her (their) concerns, allow her (them) to express herself (themselves) about the desire for a child and to support her (them) in the difficult choice.
It is important to underscore, however, that the counselling described here does not provide and/or replace any form of long-term psychological assistance, which should be offered whenever it appears necessary in cancer patients. The counselling described here has a different, timelier objective. It is meant to offer guidance and assistance through a particularly stressful decision-making process brought about by the urgency of cancer treatment.
Many studies have shown that information on fertility preservation methods is insufficient. From these accounts we learn that at least half of the patients have no memory of a discussion of fertility at the time when their treatment was instituted [11–14]. These studies also outline that when patients receive advice it tends to be qualitatively and quantitatively insufficient [16–19]. The American Society of Clinical Oncology Recommendations on Fertility Preservation in Cancer Patients require the oncologist to routinely offer a referral for psychological counselling if a man or woman has moderate to severe distress about potential infertility [20].
To conclude, ad hoc counselling is necessary for all patients confronted with cancer during their reproductive life. This is primarily intended to provide clear and precise information on ART and discuss all existing options, including cryopreservation of oocytes, PNs or ovarian tissue or refusal of fertility preserving methods. Generally speaking, such counselling offers support for young women or couples confronted with stressful cancer and fertility issues and helps them through their sometimes difficult decision-making process.
Close collaboration between the different therapeutic teams involved (onco-gynaecologists, oncologists, radiotherapy specialists, ART specialists and counsellors) is of the utmost importance.
Counselling on treatment and fertility preserving options in various cancers requires a multidisciplinary approach, as proposed by the Cancer and Fertility Task Force (Réseau Romand) in French-speaking Switzerland ( http://www.grssgo.ch ). The number of cancer patients undertaking an emergency ART programme is steadily growing with increasing awareness of the potentialities and medical progress.
Until now, we have not conducted systematic interviews with validated questionnaires to assess patients’ evaluation of counselling, and we are considering starting this in the future. But the feedback from young cancer patients has been very positive and indicates that our counselling is of great help and assists them in their decision-making, thus confirming the importance of offering specific counselling to patients or couples confronted with cancer and fertility issues within the restricted time interval between the diagnosis of cancer and the beginning of fertility-impairing treatments (chemo- and/or radiation therapy). In centres offering ART, which symbolises hope, the counselling should be systematically carried out by doctors or counsellors trained in medically assisted procreation counselling [6, 21]. The present description of our method may therefore serve other institutions by sparking this often forgotten need and helping some to develop their own approach.
1 http://www.grssgo.ch; http://www.espacecancer.chuv.ch
2 Réseau Romand de Cancer et Fertilité : Recommandations, 2009: Cancer du sein et fertilité, cancer de l’ovaire et fertilité, cancer du col et de l’endomètre, lymphomes et leucémies. Available from: http://www.grssgo.ch
3 Zaman K, Ambrosetti A, Perey L et al. Cancer du sein chez la jeune femme: traitements adjuvants et désir de grossesse. Rev Med Suisse. 2007;3:1298–304.
4 Rogers C, Farson R. Active listening. In Kolb D, Rubin I, MacIntyre J (eds). Organizational Psychology, 3rd edn. New Jersey: Prentice Hall, 1979.
5 Miller WR, Rollnick S. Motivational Interviewing. Preparing People for Change. New York: Guilford Press, 2002.
6 Béran M.D et Germond M. L’entretien d’évaluation des ressources psychosociales en médecine de la reproduction. Etude pilote d’une nouvelle approche: le “bilan des ressources”. J Gynecol Obstet Biol Reprod. 2000;29:662–7.
7 Emery M, Béran MD, Darwiche J, Opizzi L, Joris V, Capel R, et al. Results from a prospective, randomized, controlled study evaluating the acceptability and effects of routine pre-IVF counseling. Hum Reprod. 2003;18:2647–53.
8 Mc Goldick M, Gerson R. Génogrammes et entretien familial. 2ème éd. Paris. EME Editions Sociales Françaises (ESF), 1995.
9 de Ziegler D, Streuli I, Vasilopoulos I, Decanter C, This P, Chapron C. Cancer and fecundity issues mandate a multidisciplinary approach. Fertil Steril. 2010;93:691–6.
10 Loi fédérale sur la procréation médicalement assistée: http://www.admin.ch/ch/f/rs/c810_11html
11 Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Knowledge and experience regarding cancer, infertility and sperm banking in younger male survivors. J Clin Oncol. 2002;20:1880–9.
12 Schover LR, Rybicki LA, Martin BA, Bringelsen KA. Having children after cancer: A pilot survey of survivors’ attitudes and experiences. Cancer. 1999:86:697–709.
13 Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer LK. Fertility issues for young adult survivors of childhood cancer. Psychooncology. 2004;13:6809–699.
14 Zebrack BJ, Mills J, Weitzman TS. Health and supportive care needs of young adult cancer patients and survivors. J Cancer Surviv. 2007;1:137–45.
15 Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 2005:23:766–73.
16 Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–83.
17 Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20:1890–7.
18 Thewes B, Meiser B, Rickard J, Friedlander M. The fertility- and menopause-related information needs of younger women with a diagnosis of breast cancer: A qualitative study. Psychooncology. 2003;12:500–11.
19 Thewes B, Meiser B, Taylor A, Philips KA, Pendlebury S, Capp A, et al. Fertility- and Menopause-Related Information Needs of Younger Women With a Diagnosis of Early Breast Cancer. J Clin Oncol. 2005;23:5155–65.
20 Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K. American Society of Clinical Oncology Recommendations on Fertility Preservation in Cancer Patients. J Clin Oncol. 2006;24:2917–31.
21 Boivin J, Kentenich H. Guidelines for counselling in infertility. ESHRE Monographs, Oxford University Press, 2002.
No external funding. No competing interests.