Figure 1
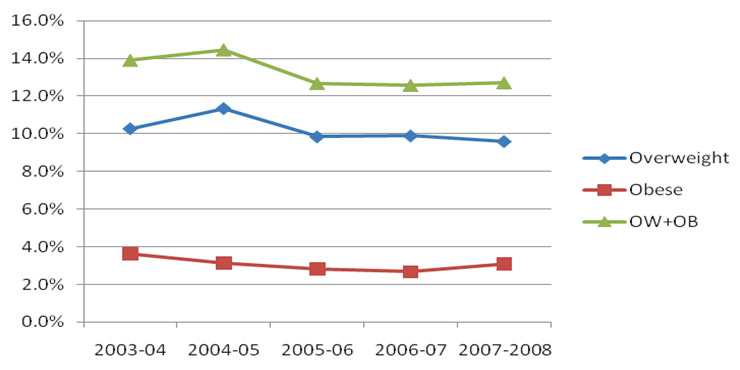
BMI over time for the entire group.
DOI: https://doi.org/10.4414/smw.2010.13040
In recent decades the prevalence of obesity and overweight has increased steadily in both developed and developing countries [1–4]. Obesity in youth has serious medium and long-term consequences including endocrine, cardiovascular, renal, pulmonary, orthopaedic and gastroenterological diseases [5, 6]. Overweight and obese youths may also face psychological challenges resulting in harm to their self-image.
For the above reasons, obesity and overweight have become a public health priority [7], particularly in school settings where the children affected may suffer stigmatisation and be confronted with learning difficulties [8].
It is therefore of interest to have robust data on the prevalence of overweight and obesity in different parts of Switzerland, to be able to monitor the effect of preventive interventions and/or regional variations.
Few longitudinal data collected in a systematic manner exist for preschool children in Switzerland. Because of the potentially important role attributed to schools in the prevention of overweight and obesity [9], it is of interest to have data on its prevalence among children entering school. This may also allow better targeted prevention programmes.
The aim of our study was to systematically weigh and measure, over a five-year period starting in 2003, 5–6-year-old children entering the Geneva public school system in order to establish their absolute and relative BMI for age.
Taking the entire group into consideration and using Cole’s references [11], there was an overall tendency towards a non-significant decrease: –0.7 points (p = 0.25) for overweight (OW) and –0.5 points (p >0.23) for obesity (O) over the 5-year study period.
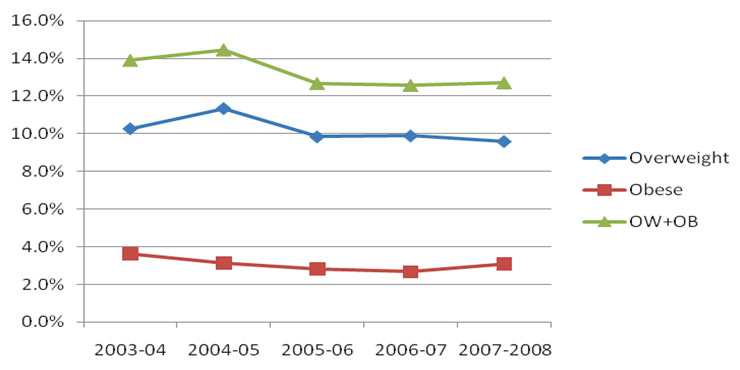
Figure 1
BMI over time for the entire group.
Following a small increase in the percentage of OW + O from 2003–4 to 2004–5 and a 1.8 point decrease from 2004–5 to 2005–6, a stabilisation has been observed in OW + O at around 12.6% (table 1 and fig. 1). When computing changes on a yearly basis we observed a significant 1.5 point decrease in overweight children between 2004–5 and 2005–6 (11.3 vs 9.8%; p = 0.033). This was not the case for obesity (3.1 vs 2.8%; p = 0.44).
When analysing boys and girls separately, girls showed a higher overall prevalence of OW + O than boys (14.2 vs 11.8%).
Over the 5-year period girls showed a larger decrease in OW (–1.1 points, p = 0.27) and O (–0.5 points, p = 0.48) than boys (OW: –0.3 points, p = 0.3; and O: –0.6 points, p = 0.73). There was no statistically significant difference for the decrease in OW and O between boys and girls (tables 2 and 3).
In view of the recommendations of the Swiss Paediatric Society we also analysed our data in an identical manner, using Kromeyer’s references (tab. 4). In so doing there was no longer a decrease in OW but a stagnation, whilst O decreased by –0.5 points between 2003–4 and 2007–8 in a similar way to Cole’s referential.
Girls showed a 0.2 point increase in OW compared to a 1.1 point decrease with Cole’s referential, but O decreased in a similar fashion (–0.5 points). Boys showed similar variations to those seen with Cole’s referential (table 4).
| Table 1Distribution of the prevalence (95% confidence intervals) divided into ISO-BMI subgroups for the entire group. | ||||||||||
| Prevalence | 2003–4 | 2004–5 | 2005–6 | 2006–7 | 2007–8 | |||||
| N = 3728 | N = 3908 | N = 3718 | N = 3709 | N = 3533 | ||||||
| ISO-BMI <25 | 86.1% | 84.9–87.1 | 85.5% | 84.3–86.5 | 87.3% | 86.2–88.3 | 87.4% | 86.3–88.4 | 87.3% | 86.1–88.3 |
| ISO-BMI 25–30 | 10.3% | 9.3–11.3 | 11.3% | 10.3–12.3 | 9.8% | 8.9–10.8 | 9.9% | 8.9–10.9 | 9.6% | 8.6–10.6 |
| ISO-BMI >30 | 3.6% | 3–4.2 | 3.1% | 2.5–3.6 | 2.8% | 2.3–3.4 | 2.7% | 2.2–3.2 | 3.1% | 2.6–3.7 |
| Table 2Distribution of prevalence (95% confidence intervals) divided into ISO-BMI subgroups for girls. | ||||||||||
| Prevalence | 2003–4 | 2004–5 | 2005–6 | 2006–7 | 2007–8 | |||||
| N = 1802 | N = 1927 | N = 1834 | N = 1775 | N = 1764 | ||||||
| ISO-BMI <25 | 84.2% | 82.4–85.8 | 83.8% | 82.1–85.4 | 86.5% | 84.8–88 | 85.6% | 83.9–87.1 | 85.8% | 84–87.3 |
| ISO-BMI 25–30 | 12.0% | 10.6–13.6 | 12.9% | 11.4–14.4 | 10.6% | 9.3–12.11 | 11.3% | 9.9–12.9 | 10.9% | 9.5–12.4 |
| ISO-BMI >30 | 3.8% | 2.9–4.7 | 3.3% | 2.5–4.1 | 2.9% | 2.2–3.7 | 3.1% | 2.3–4 | 3.3% | 2.6–4.2 |
| Table 3Distribution of prevalence (95% confidence intervals) divided into ISO-BMI subgroups for boys. | ||||||||||
| Prevalence | 2003–4 | 2004–5 | 2005–6 | 2006–7 | 2007–8 | |||||
| N = 1926 | N = 1981 | N = 1884 | N = 1934 | N = 1769 | ||||||
| ISO-BMI <25 | 87.9% | 86.4–89.3 | 87.2% | 85.7–88.6 | 88.2% | 86.6–89.6 | 89.1% | 87.7–90.4 | 88.8% | 87.3–90.2 |
| ISO-BMI 25–30 | 8.6% | 7.4–9.9 | 9.8% | 8.5–11.1 | 9.1% | 7.8–10.4 | 8.6% | 7.4–9.9 | 8.3% | 7–9.6 |
| ISO-BMI >30 | 3.5% | 2.7–4.4 | 3.0% | 2.3–3.8 | 2.8% | 2.1–3.6 | 2.3% | 1.7–3 | 2.9% | 2.2–3.7 |
| Table 4Distribution of prevalence using Kromeyer’s references for the entire group and divided into gender subgroups. | ||||||
| 2003–4 | 2004–5 | 2005–6 | 2006–7 | 2007–8 | ||
| Entire group | Overweight | 5.7% | 7.3% | 5.8% | 6.3% | 5.7% |
| Obese | 3.9% | 3.4% | 3.0% | 2.9% | 3.4% | |
| Girls | Overweight | 5.4% | 7.6% | 5.3% | 6.0% | 5.6% |
| Obese | 3.8% | 3.1% | 2.8% | 2.9% | 3.3% | |
| Boys | Overweight | 6.0% | 6.9% | 6.3% | 6.5% | 5.8% |
Despite worrying international trends in childhood OW and O [7, 14], our study showed no further rise in the prevalence of OW and O after 2005 in 6-year-old children living in the Canton of Geneva (both with Cole’s and Kromeyer’s references). On the contrary, a small non-significant decrease in OW and O was observed after 2005 and has stayed constant since (Cole’s referentials).
Compared to some other studies from Switzerland, our data tend to show relatively lower levels of OW and O [15, 16].
However, when comparing our data with the data collected on whole population samples of similar-age children in the cities of Bern, Basel and Zurich [17], the trend and the values are very similar and seem to confirm the trend in large Swiss cities. It must be borne in mind that the prevalence of OW and O may vary between different geographical areas and between urban and rural areas.
Our data also corroborate results found in Swedish 10-year-old children from the Stockholm area, where a similar decrease in the prevalence of OW and O was shown between 1999 and 2003 [18]. Obesity levels in both boys and girls were relatively similar to those found in our 5–6-year-old children (boys: 3.5 vs 3.8%, girls: 3.8 vs 2.8%) but the prevalence of OW was considerably higher in their group of 10-year-old children (boys: 8.6 vs 20.5%, girls: 12 vs 19.2%). This could be due to the increasing prevalence of O and OW with age.
A similar trend was also observed in the Bordeaux area where the Programme National Nutrition Santé (PNNS) is implemented. A significant 3.1% (p <0.01) decrease in OW + O in 6-year-old children between 2005 and 2007 was reported [19].
Globally there seems to be a trend in OW and O in certain areas of Europe towards a clearcut levelling of the “epidemic” or even an improvement. These are encouraging data even though the underlying causes of the change are not yet clear. The hypotheses range from the effect of prevention and public awareness to a change in body image. One could also hypothesise that the genetic susceptibility (tendency to gain weight) of the population in these areas has struck a balance with the “obesogenic” effect of the environment to which they are exposed, even though this will be difficult to prove.
The fact that the BMI change in Bordeaux was of a similar magnitude and at exactly the same time (2004–5 to 2005–6) in both Geneva and Bordeaux is intriguing. Interestingly, comparing the average temperature for the 4 winter months in both areas shows that the 2 winters preceding the decline in BMI were significantly colder than the average. Could this be a thermogenic effect due to low outdoor temperatures, which is known to stimulate brown fat, as proposed by Farmer [20]? Could it be that global warming is contributing to a progressive decrease in the stimulation of brown fat, thus leading to a drop in basal metabolism? Are we overheating our homes and overdressing our children? All these questions may well be related to the current trend in OW and O. Further research will be needed to clarify this.
Even though socio-economic differences were not evaluated in our study, both previous research [21] and the studies by Sundblom and Ruello [18, 19] underline the important effect socio-economic factors have on the prevalence and evolution of OW and O. Special attention should be paid to these groups if long-term solutions are to be found for this problem.
When comparing boys to girls, girls showed a higher prevalence of OW and O than boys, as described in the literature. Girls, however, showed a larger, non-significant, decrease in OW and O over the 5-year period. A clear explanation for this is difficult to find bearing in mind the young age group, where conscious behaviour changes are improbable. Parental preoccupation with the girl’s future morphology may be of interest compared to boys, in whom corpulence may be an asset at this young age.
This is encouraging data even though the prevalence of OW and O at school admission (12.6%) can be considered relatively high and warrants an early-age approach to the problem. All approaches touching pre-school children, such as perinatal information, day-care interventions (nutrition, physical activity) and parental advice, should be strongly encouraged.
Comparing the two referentials (Cole, Kromeyer) underpins the major differences found in the prevalence of OW and O, depending on which references are used. A 4% difference was found for OW and 0.35% for O.
Obesity has many implications for children’s health. It is therefore important that youth health departments participate in the early detection and prevention of OW and O.
Preventive approaches have shown some success, especially when whole community approaches are adopted [22]. Considering the difficulties in inducing behavioural changes, structural approaches such as limiting of access to certain foods and generating a health-promoting environment must be encouraged [9, 23].
In conclusion, the data collected between 2003 and 2008 among 18 596 5–6-year-old children in Geneva show a non-significant decrease in the prevalence of O and OW (Coles’s references). This finding corroborates findings in other cities in Switzerland, Sweden and France and may be among the first signs of a changing trend in O and OW. The relatively high level of O and OW at 5 years of age, however, merits special attention in that 13–14% of children already fall into the O and OW groups. Even if no clear conclusions can be drawn as to the reasons for this change, it is probable that both environmental and individual factors contribute to influencing people’s behaviour. An intriguing finding was the concomitant drop in O and OW in both Bordeaux and Geneva between 2004–5 and 2005–6. There seems to be a link between particularly cold winters and the drop in BMI. The influence of environmental temperature on brown fat metabolism may be of interest for future research.
1 Jackson-Leach R, Lobstein T. Estimated burden of paediatric obesity and co-morbidities in Europe. Part 1. The increase in the prevalence of child obesity in Europe is itself increasing. Int J Pediatr Obes. 2006;1:26–32.
2 Lobstein T, Jackson-Leach R. Estimated burden of paediatric obesity and co-morbidities in Europe. Part 2. Numbers of children with indicators of obesity-related disease. Int J Pediatr Obes. 2006;1:33–41.
3 Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5.
4 Pomerleau J, McKee M, Lobstein T, et al. The burden of disease attributable to nutrition in Europe. Public Health Nutr. 2003;6:453–61.
5 Singhal A. Endothelial dysfunction: role in obesity-related disorders and the early origins of CVD. Proc Nutr Soc. 2005;64:15–22.
6 Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res. 2005;13:163–9.
7 Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50.
8 Viguie M, Fayard M, Micheletti P, et al. Prevalence of obesity amount elementary school children in Grenoble. Sante Publique. 2002;14:361–70.
9 Davis MM, Gance-Cleveland B, Hassink S, et al. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–S253.
10 Dayer-Métroz M, Mermillod B, Pampallona S, Schopfer C. Croissance somatique de 2 à 18 ans – courbes genevoises 1995 – étude transversale. Service Santé de la Jeunesse, Genève; 1995.
11 Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
12 Kromeyer K. Growth in body height by children between 4 and 12 years of age – results of the Jena longitudinal study. Anthropol Anz. 1994;52:327–40.
13 Finne E, Reinehr T, Schaefer A, et al. Overweight children and adolescents – is there a subjective need for treatment? Int J Public Health. 2009;54:112–6.
14 Seidell JC. Obesity in Europe: scaling an epidemic. Int J Obes Relat Metab Disord. 1995;19(Suppl 3):S1–S4.
15 Woringer V, Schutz Y. Obesity in Switzerland: body mass index (BMI) percentiles of a child and adolescent population born in 1980 in Lausanne and comparison with Swiss norms (1955). Soz Praventivmed. 2003;48:121–32.
16 Zimmermann MB, Gubeli C, Puntener C, et al. Overweight and obesity in 6–12 year old children in Switzerland. Swiss Med Wkly. 2004;134:523–8.
17 Promotion Santé Suisse. Indicateur pour le domaine «Poids corporel sain». http://www.gesundheitsfoerderung.ch/pdf_doc_xls/f/Gesundes_Koerpergewicht/Grundlagen_Wissen/Monitoring/Indikatoren/Bericht-Indikatoren-Juni_2009_f.pdf 1-6-2009.
18 Sundblom E, Petzold M, Rasmussen F, et al. Childhood overweight and obesity prevalences levelling off in Stockholm but socioeconomic differences persist. Int J Obes. (Lond) 2008;32:1525–30.
19 Ruello M, Thibault H. Programme for Nutrition,Prevention and Health of children and teenagers in Aquitaine, France. WHO meeting on community interventions to improve nutrition, Berlin, February 21–22nd, 2008.
20 Farmer SR. Obesity: Be cool, lose weight. Nature. 2009;458:839–40.
21 Magnusson MB, Hulthen L, Kjellgren KI. Obesity, dietary pattern and physical activity among children in a suburb with a high proportion of immigrants. J Hum Nutr Diet. 2005;18:187–94.
22 Kumanyika S, Jeffery RW, Morabia A, et al. Obesity prevention: the case for action. Int J Obes Relat Metab Disord. 2002;26:425–36.
23 Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794-e802.
No conflict of interest in relation to this article.