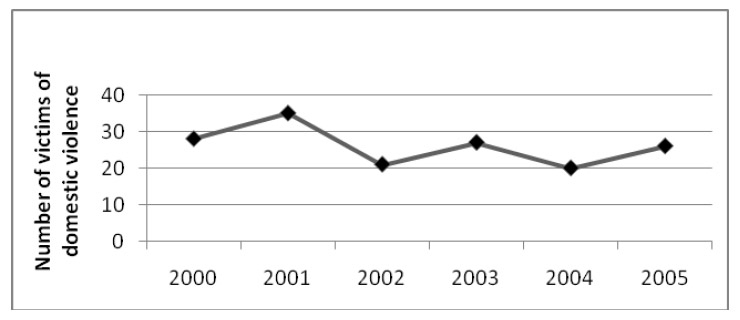
Figure 1
Identified cases of domestic violence per year from 2000 to 2005.
DOI: https://doi.org/10.4414/smw.2010.13047
Domestic violence is a major public health problem [1–4]. Several studies have reported a prevalence of 6–30% for women treated for abuse-related symptoms at emergency departments (ED) [4, 5]. A systematic literature review shows that at least 6% of ED patients in the United Kingdom have experienced domestic violence within the previous 12 months [6]. The authors estimate a higher prevalence of domestic violence amongst ED patients than in the general population. A study published in 2004 by the Federal German Health Department recorded that 25% of all women questioned had been victims of domestic violence, in one third of them serious, i.e. involving multiple body injuries [4]. A representative inquiry conducted among patients in a Swiss obstetric clinic [3] showed that every fourth woman had been victim of violent abuse in an intimate relationship. Moreover, estimates suggest that 22–35% of injured women admitted to an ED had suffered these injuries through violent partner abuse [7]. Although the medical significance of domestic violence has been epidemiologically affirmed, medical experts still underestimate the phenomenon and are partly unaware of it [8, 9]. Several studies record medical neglect of this theme [8–10].
In Switzerland, data concerning victims of general violence treated at emergency departments have indeed been collected, but no report on the prevalence of domestic violence in an emergency department has so far been published [11, 12]. Also, few studies exist in German-speaking countries on the quality of medical documentation of injuries from a forensic viewpoint [13]. The present study is intended to show whether, and to what extent, domestic violence is identified as such in an urban Level 1 emergency department, whether the figures collected correspond to data in recent international studies, and whether the related documentation meets the quality requirements of forensic medicine.
The American Medical Association’s definition of domestic violence includes: “a pattern of coercive behaviours that can include battering and injury, sexual assault, social isolation, deprivation, and intimidation perpetrated by someone who was or is intimate with the victim” [1]. Thus domestic violence is neither solely a medical diagnosis nor an element of a crime, but more a phenomenon that equally concerns the medical professions, law enforcement, social workers and others.
The emergency department at the University Hospital of Berne is the only Level 1 accident and emergency unit for adults (>16 years of age) in this area providing service for all social classes and insurance groups. Approximately 12 000 women are admitted annually to the emergency department.
The data were collected retrospectively from 1 January 2000 to 31 December 2005 using the emergency department software QualicareTM (Qualidoc, Trimbach, Switzerland). The software is able to connect clinical data with classified key words, thus allowing immediate search for e.g. patient groups with a particular diagnosis, such as “domestic violence”.
All reports of female patients in the above-mentioned period were automatically scanned for the following key words, corresponding to the usual definitions of physical violence [2, 3]: “Gewalt” (Eng.: violence), “Stossen” (to push), “Schläge” (blows), “schlagen” (to hit), “Jochbein” (cheekbone), “Würgen” (strangulation), “Kopfverletzung” (head injury), “Schütteln” (to shake), “Schuss” (shot), “Stichverletzung” (stab wound), “stumpfes Trauma” (blunt trauma), “Gesichtsverletzung” (facial injury). We searched for key words most likely to reflect physical domestic violence. All reports showing a present or former relationship to the perpetrator, a family member or a near acquaintance to the victim, or documenting explicit domestic violence as a cause of ED admission, are included in the study. Age, marital status, type of relationship, type of admission to the ED, location and cause of violence, injury pattern, classification of the injuries (Swiss penal code), drug and/or alcohol influence, type of treatment (inpatient or outpatient), further investigations and interventions, duration of disability, were reported. If a patient has been seen more than once, each visit counted as one.
Forensic medicine documentation differs from “normal” medical documentation in a number of decisive respects. The latter actually consists primarily of registration of the treated patient in the form of a case history. Apart from being required by law, the aim of this documentation is to provide a comprehensive report, from the patient’s history all the way through to diagnosis and further procedures for diagnosis and therapy. On the basis of the medical record it should always be possible to comprehend the manner in which the physician was assigned to the patient, what steps were taken to establish a diagnosis and what therapeutic measures were taken. Further, the information process from physician to patient must be documented.
The forensic medicine documentation is a constituent part of a medical record as well as of any available court minutes [14, 15]. Such documentation is established in case the findings on the patient’s body are obviously or possibly related to an offence, or if a court order has been issued. It should both meet the general standards for a medical record and meet the needs of criminal proceedings. Experience and the literature show that this quality of the documentation varies considerably [15, 17, 18]. Standardised forensic medicine documentation is important for the purpose of legal equality and ensuring quality for victims of violence who receive medical certificates. Criminal investigation of victims of violence includes clarification of the following questions [14, 16]:
1. Has an offence been committed (self-inflicted or external agency, accident)?
2. Extent of injuries (classification)?
3. “Age” of the injuries (how long ago were they inflicted?)
4. Cause of injuries, presumption of a instrument
In court proceedings, an expert should be able to give evidence on the above-mentioned questions without having examined the victim himself and only by studying the medical documents. Documentation should comprise the following information:
1. Personal data
2. History, e.g. information on the circumstances of the offence.
3. Injuries:
a. Type (bloodshot, laceration, etc.)
b. Localisation
c. Extent, size, dimension,
d. “Age” of the injury
e. Shape
Explanation on item 3:
a.) Indications of the “type of injury” were considered complete when a diagnosis was stated in the report (e.g. bruise, cut, scratch) or when the wound morphology, i.e. the wound’s edges, base, surrounding, allowed a wound diagnosis to be established.
b.) Description of wound localisation was considered sufficient when the injured part of the body could be located.
c.) Indications of size are met when the unit of measurement is given (usually cm)
d.) For this study, the wound’s “age” is considered defined if it is evaluated in the report (recent, old, etc.) or if the wound’s description allows a conclusion to be drawn.
e.) The shape is considered given with a bi-dimensional description of an injury or with concrete indications of the shape.
One point is attributed for each item fulfilled, i.e. a complete report from the forensic medicine viewpoint scores 5 points.
In order to obtain the highest score, photos and sketches must show the following: localisation, colour, extent and shape of the findings.
Fulfilment of these criteria scores a maximum of 4 points.
Complete documentation can thus score a maximum of 9 points, provided the general conditions for establishing a medical case history are fulfilled.
From 2000 to 2005 a total of 40 914 women were admitted to the ED. Based on the ED reports we identified a total of 161 victims of domestic violence, an average of 26.5 victims per year (SD15) and 6819 female ED patients per year over the six-year period (see fig. 1). We included 160 cases of domestic violence that met our inclusion criteria.
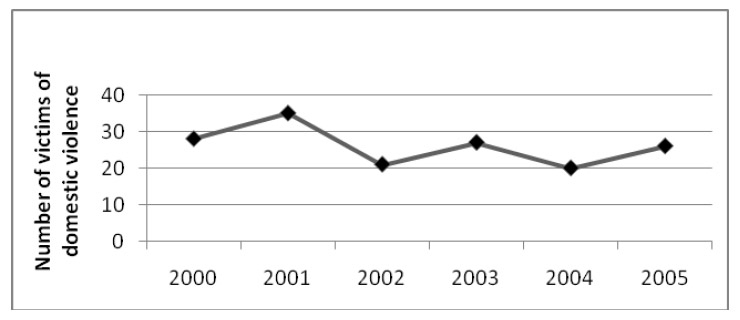
Figure 1
Identified cases of domestic violence per year from 2000 to 2005.
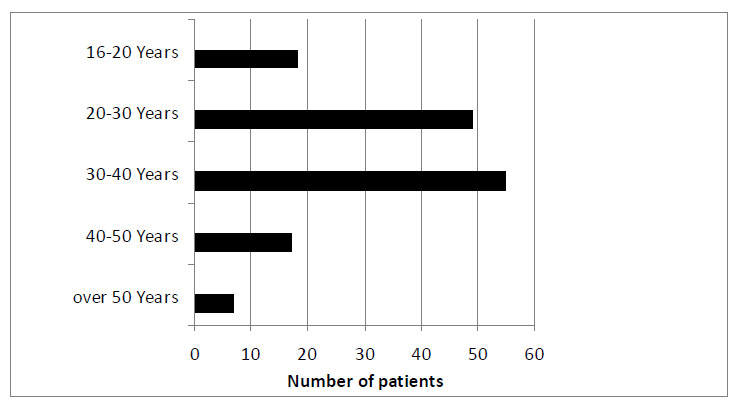
Figure 2
Age of the patients.
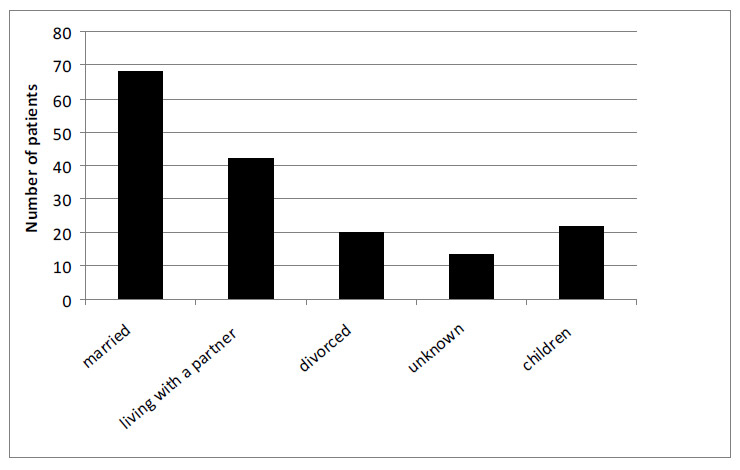
Figure 3
Sociodemographic data.
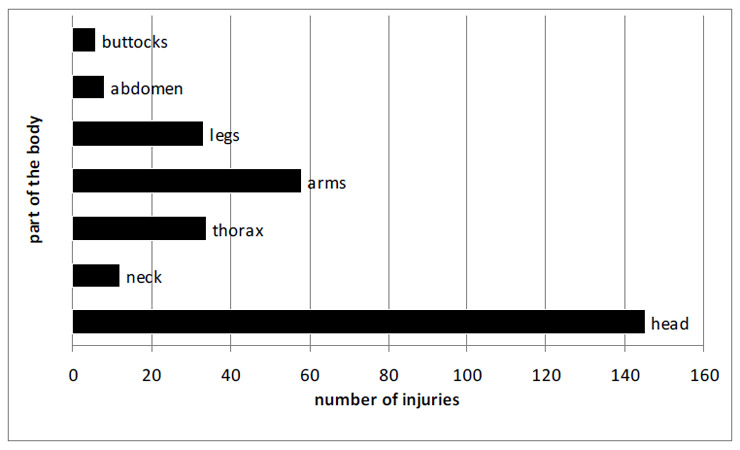
Figure 4
Injuries on different parts of the body.
Age and ED visits: Basically, all age groups are concerned – the oldest patient was 68, the youngest 15. However, occurrence of violence was most frequent among relationships in the reproductive or family phase, i.e. between the ages of 20 to 50, with a peak at 40. During the study period, nine women were examined twice, one woman was examined three times and another four times (see fig. 2).
Social status and ED visits: Basically, demographic data were sparse in the reports. Almost two thirds (63.6%) of all women concerned are married or live in a steady relationship (see fig. 3).
Weekly distribution and time of ED visits: There is a conspicuous accumulation of domestic violence-related visits at weekends; almost half (46%) of all cases occur on Friday, Saturday and Sunday. The scattering over the different times of the day also displays the occurrence of domestic violence at times when men are usually at home. Nevertheless, in more than half of the cases examined the time of occurrence remained unspecified in the reports.
Mode of reference: More than two thirds (65%) of all cases were self-referred. 7% were GP-referred or clinic-referred, 12% were delivered by ambulance and 7% by the police. Basically, the mode of reference does not allow conclusions as to severity of injury. Nevertheless, it is noticeable that bodily pain is in the foreground among patients delivered by rescue services, and is often medically more serious than that of self-referred patients.
Type of violence and location of injuries: For most of the cases (70.2%), blunt violence was documented in the form of bloodstains, scratches, bruises, lacerations and, in rare cases, bone fractures. Pressure-induced pain was described in 57 cases (12.9%). Although this sign is usually a sequel to blunt violence, it was not considered in evaluating blunt violence injuries since it is a subjective finding. In 49% of cases signs of blunt violence were to the head, most often in the eye region (15.5%), to the mouth (8.8%) and the jaw (7.4%). Upper extremities were injured in 19.6%, lower extremities somewhat less frequently in 11.1%. The majority of cases, 53%, showed injuries to only one body area, 22% in 2 and 25% to more than 2 body areas. The instruments causing the injury were fist blows in 72% of cases and kicks in 14%. The effect of objects used as weapons was described in 15 cases, no detailed indication being given as to the weapon. Sharp violence is described in 9 cases, of which 7 showed one injury and 2 cases injuries on 2 localisations. The arms were in most cases (5 cases) injured. Sexual violence is described in 4 cases (see fig. 4 and 5).
In 10 cases strangulation has been claimed. A strangulation mark is documented in all cases. In 3 cases, petechial haemorrhage in the conjunctiva is described. In one of these cases, a forensic medicine specialist was consulted.
Classification of injuries (Swiss penal code): As regards Swiss criminal law, 75% of the assaults can be classified as simple assault, namely when there is no evidence of danger to life, of mutilation, severe deformation or other severe damage to a person’s health (see fig. 6).
Psychiatric comorbidity: 8 women showed an acute suicidal tendency; in 31 of the cases examined a psychiatrist was called for consultation. Altogether, 16 women showed no injury and were examined solely following psychiatric decompensation in the context of domestic violence.
Perpetrator: In 3/4 of the cases (64.4%), the husband or partner was reported as perpetrator, in some 10% (9.4%) the former partner, in 26.1% other family members or no documentation. The perpetrator was under the influence of alcohol in 16 cases and under drug influence in 7 cases. In 15 cases, victims were described as under the influence of alcohol.
Disability and hospitalisation after ED stay: Total disability was described in 17% of cases, no disability in 8.1%; in 75% of cases the disability is not defined on the basis of reports.
73% of the female patients examined were discharged from the ED after examination, 14 women were hospitalised and the rest were transferred to other clinics or to a psychiatrist. Altogether, 22 female patients (barely 14%) received psychiatric treatment. 20.8% were referred to a victim aid programme.
Semi-quantitative analysis of the forensic medicine documentation: Only the cases with documented injury (n = 141) were considered for this evaluation. In 12 cases, according to the report, the ED’s medical staff photographed the injuries; in 4 cases, the Forensic Medicine Institute prepared a photographic record of the findings. At the time of our analysis, none of the photos taken by the ED’s staff could be found, and hence analysis of documentation quality is confined to the written reports. The types of injuries were described in all cases and their localisation in 96%. A declaration was made to the lesion’s “age” in 12% of the cases, to its shape in 26% and to its extent in 36%. Only 7 cases reached the highest score of 5 for the written report, i.e. met the forensic medicine requirements described above. 29 reports scored 4, the indications as to the injury’s “age” being largely missing; a score of 3 was assigned to 21 reports, of 2 to 79 reports (56%) and of 1 to 3 reports (see fig. 7).
Altogether, 135 doctors were involved in the cases we assessed, of whom 57 were assistants and 21 students conducting the examinations under the supervision of a senior physician.
The present retrospective assessment of medical reports over a period of 6 years shows an average proportion of 0.4% documented female patients affected by domestic violence. This figure is far below the proportions to be expected from more recent data. In her literature review Olive [6] notes a minimal prevalence of 6% of ED patients; other studies report prevalence between 6–30% of female ED patients; in a prospective analysis Dearwater [5] finds 2.2% of an ED’s injured female patients to be victims of domestic violence. Studies on the prevalence of domestic violence among the population worldwide report that every 4th to 5th woman could be affected by domestic violence [1–4]; according to this the proportion in our study appears too small. It is possible that, due to the setting’s limitations, not all reports underwent assessment, or it must be admitted that the majority of domestic violence cases are not registered in the daily medical round. Underestimation of domestic violence is a known phenomenon [9]. Several studies estimate that without screening, a large proportion of victims go unidentified [7, 18, 26]. In fact, screening is recommended not only where suspicion of domestic violence exists (suspicion screening), but also of all patients [6]. An opportune intervention ensures both an improved health outcome and enhancement of social competences [6, 20]. Recent studies attest that screening in EDs has no adverse effects, and that a consistent network allows better exploitation of resources for the persons concerned [26]. A prospective analysis in the form of screening at the Inselspital ED is the logical consequence of the present study; it is certainly the only means of determining whether there are indeed fewer domestic violence victims in Bern or whether domestic violence is underestimated from a medical point of view and thus remains unidentified.
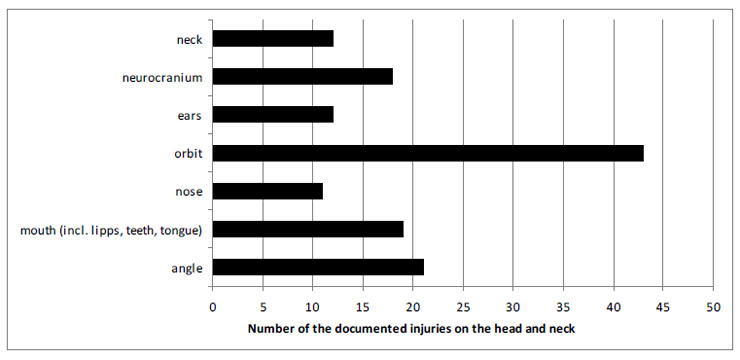
Figure 5
Localisation of the injuries in the region of the head and neck.
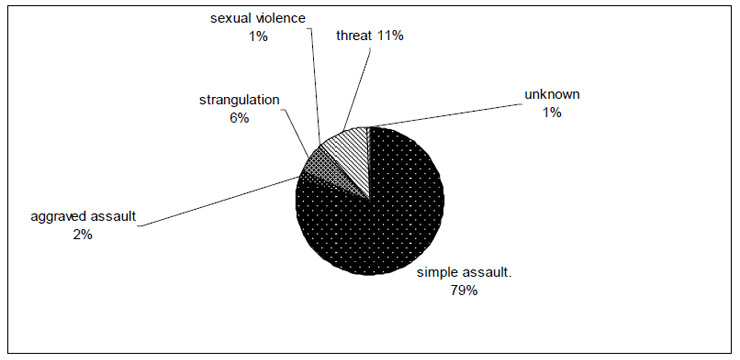
Figure 6
Legal classification of the assaults, according to the Swiss penal code.
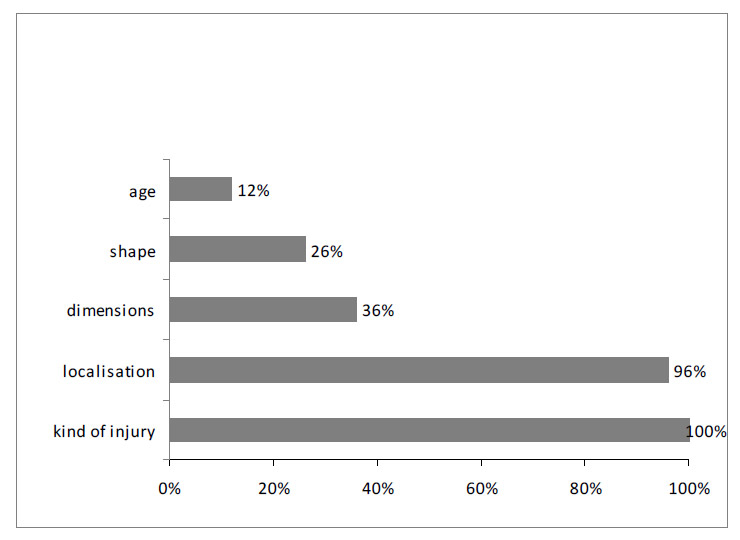
Figure 7
Semiquantitative analysis of injuries in the medical reports concerning forensic aspects.
Nearly 70% of the documented injuries result from blunt violence, chiefly subsequent to fist blows, more seldom from kicks. The current partner is pointed out as the perpetrator in some 74% of cases and the former partner in 10%. The reports point out the effect of weapons as the cause of the injuries in only 10% of the cases, no detailed indication being given as to the weapon. With 49% of the cases the head, especially the facial region, was the most frequently affected area. Due to the search method, these results are liable to a certain bias and thus should be discussed with care. They coincide with various data, i.e. of Fanslow [21] and Allen [23], who found that victims of assault-related injuries often displayed blunt violence injuries and showed 13 times more head injuries than unintentional injury victims. Exadaktylos et al. also report an accumulation of head injuries resulting from perpetrated blunt violence, in most cases indeed through the use of weapons [11]. It remains doubtful whether the localisation and type of injuries alone can be considered as predictor or indicator of assault-related injuries [21, 23], the predictive value being too slight [21]. According to Allen et al. [23], localisations of injuries in relation to the injured person’s age could indeed be significantly predictive. He classified the body into different areas and found that central areas such as head, neck and chest more frequently displayed wounds resulting from assault-related injuries in comparison to limbs more often accidentally injured. From the forensic medicine perspective arm injuries deserve particular attention as probable defence injuries. Indeed, in 20% of cases we still found an associated injury of the upper limbs, especially in the rarely documented case of injuries from a sharp instrument such as a knife or scissors. Recognising ostensible defence injuries is pertinent, since from them, under certain circumstances, the victim’s defence and resistance behaviour can be defined [15].
Partner violence seldom leads to severe injuries in the penal sense of the term. According to Swiss law a severe injury is defined as one which endangers life, or if, in the case of mutilation, disfigurement or lasting impairment can be expected.
Among our group of patients, and on the basis of the available records, we defined 80% of the injuries as not severe. The threat of prosecution is thus to be considered slight for these cases. This is particularly to be considered in the context of amendments to Swiss penal law, according to which ostensible simple bodily harm would usually be punishable with fines. Thus it is questionable whether penal law measures can do justice to the biopsychosocial collateral harm caused by domestic violence, such as, for example, psychosomatic disorders and other stress-related damage [3, 5, 22].
In 10 cases strangling was claimed and in each case strangulation marks were visible. Strangulation is considered a danger to life if petechial haemorrhages can be proven in the facial skin including eye conjunctiva and other mucous membranes [24]. These are signs of an at least short-term significant interruption of blood flow in the carotid arteries. Such petechial haemorrhages were documented in 3 out of these 10 cases. From the viewpoint of forensic medicine even the absence of such haemorrhages is significant. The legal consequences are important in certain circumstances, as a Federal court judgement rendered in 1998 (BGE 124 IV 53, 1998) shows. In doubtful cases, it is recommended that a forensic specialist be called if possible.
Given our scoring system, the evaluation of the medical documentation from a forensic perspective is relatively crude and not validated, although it definitely reveals a trend.
On the basis of the documents inspected, a secondary assessment, i.e. in the framework of a court procedure, would not be feasible from the viewpoint of forensic medicine, since indications as to the size of the injuries are missing in two thirds of the cases, indications as to the shape in 74% and as to the “age” in 88%. It was not possible, for example, to draw a definite distinction between an accidental and a violence-related event, or to draw a conclusion as to a possible weapon. The photos that have been made – in fact in 12 cases only – are also missing, and it is thus not possible to verify whether the stated type of injury, for example scratch or contusion, actually is such an injury in the context of forensic medicine. Neglecting the quality of the forensic documentation cannot be attributed solely to just a few practitioners, as is shown by the participation of 135 doctors in putting the records together. Also, similar deficiencies have already been described elsewhere [14, 26]. It is quite understandable that, in the midst of a busy ED’s hectic activity, superfluities are avoided. Notwithstanding, a particularly careful documentation would prove worthwhile in cases where interpersonal aggression is obvious or suspected [13–15, 17]. Interestingly enough, the “age” of the injuries was assigned particularly little importance in the cases assessed. The description allowed deduction of a lesion’s “age” in only 12% of the cases. This is significant, since later on it is not possible to distinguish several injuries suffered at different times. Nor is it possible to corroborate injuries documented without these indications with allegations by the victim or perpetrator as to the moment of the injury. The size and shape of the injuries did indeed receive somewhat more attention, though still in a minority of cases. This data is significant in drawing conclusions as to a likely weapon or the violence of the abuse [13, 15]. The assessment indubitably shows a need for education and continuing education of practitioners in the field of forensic medicine and its documentation. The introduction of standardised documentation forms, for example from the Internet, is also recommended. Photos are today an important feature of medical documentation, and it is recommended that these photos be consigned to case-specific storage, possibly in a special picture database.
A consequence of the present study should be validation of the suggested documentation score, allowing quality control that is both more solid and of wider scope from the perspective of forensic medicine.
This study observed only one ED in a large university hospital. More centres should be investigated in order to ensure that the conclusions drawn here are valid for Swiss EDs in general. The validation of the score used in the present study is crucial in forging a better instrument to analyse the quality of documentation in forensic medicine. The present study underlines the likelihood that some cases are overlooked. A prospective study should be undertaken to reveal the evidence of a significant impact on health and to fathom the extent of the problem. However, ethical obstacles have shown themselves a major problem.
– Domestic violence screening should be introduced for improved detection.
– Increased awareness is needed and a search for non-accidental event genesis, especially in the presence of face, neck and arm injuries.
– Claimed strangulation should be investigated with particular care from the perspective of forensic medicine.
– Penal legal norms for domestic violence should be investigated at least in Switzerland as to their validity and eventual preventive impact.
– Practitioner education and continuing education should be intensified in forensic medicine documentation.
– Photographic documentation of the cases should be stored.
1 American Medical Association. Diagnostic and treatment Guidelines on Domestic Violence. 1992
2 Gillioz L, De Puy J, Ducret V. Domination et violence contre la femme dans le couple. Nationalfondsstudie, Lausanne 1997.
3 Gloor D, Meier H. Frauen, Gesundheit und Gewalt im sozialen Nahraum. Repräsentativbefragung bei Patientinnen der Maternité Inselhof Triemli. Büro für die Gleichstellung von Frau und Mann der Stadt Zürich und Maternité Inselhof Triemli, Edition Soziothek Zürich, April 2004.
4 Bundesministerium für Familie, Senioren, Frauen und Jugend, Prof. U. Müller, M. Schröttle, S. Glammeier. Lebenssituation, Sicherheit und Gesundheit von Frauen in Deutschland – eine repräsentative Untersuchung zu Gewalt gegen Frauen in Deutschland. Berlin, 2004.
5 Dearwater StR, Coben JH, Campell JC, Nah G, Glass N, McLoughlin E, Bekemeier B. Prevalence of intimate Partner Abuse in Women Treated at Community Hospital Emergency Departments. JAMA. 1998;280:433–8.
6 Olive Ph. Care for emergency department patients who have experienced domestic violence: a review of the evidence base. J Clin Nurs. 2007;16(9):1736–48.
7 Halpern LR, Perciaccante VJ, Hayes C, Susarla S, Dodson TB. A protocol to diagnose intimate partner violence in the emergency department. J Trauma. 2006;60(5):1101–5.
8 Flitcraft A. Clinical violence intervention: opportunities and barriers. Bull N Y Acad Med. 1996;73(1):124–9.
9 Elliott L, Nerney M, Jones T, Friedmann P. “Barriers to Screening for Domestic Violence”. J Gen Intern Med. 2002;17:112–6.
10 Zink T, Regan S, Goldenhar L, Pabst S, Rinto B. Intimate Partner Violence: What are Physicians Perceptions? JABFP. 2004;17(5):332–40.
11 Exadaktylos AK, Häuselmann St, Zimmermann H. Are times getting tougher? A six-year survey of urban violence-related injuries in a Swiss university hospital. Swiss Med Wkly. 2007;137:525–30.
12 Hofner MC, Python NV, Martin E, Gervasini J-P, Graz B, Yersin B. Prevalence of Victims of Violence Admitted to an emergency department. Emerg Med J. 2005;22:481–5.
13 Pollak St. Rechtsmedizinische Aspekte bei der Untersuchung und Dokumentation von Körperverletzungen. in: Madea, Praxis der Rechtsmedizin 2. Auflage, Springer Medizin Verlag Heidelberg, 2007.
14 Sheridan DJ. Forensic Documentation of battered pregnant women. Journal of Nurse-Midwifery. 1996;41:467–72.
15 Klopfstein U, Streit S, Schön C. Körperliche und sexuelle Gewalt an Erwachsenen: Vom forensischen Denken und ärztlichem Handeln. Ther Umsch. 2008;65:371–9.
16 Eberlein-Gonska M. Qualitätssicherung – nach wie vor nebulöse Qualität. Deutsches Ärzteblatt, Jg. 104, Heft 38, September 2007
17 Magnussen L, Shoultz J, Oneha MF, Hla MM, Brees-Saunders Z, Akamine M, Talisayan B, Wong E. Intimate Partner Violence: A Retrospective Review of Records in Primary Care Settings. J Am Acad Nurse Pract. 2004;16(11):502–12.
18 DeLahunta EA. Hidden Trauma: the mostly missed diagnosis of domestic violence. Am J Emerg Med. 1995;13(1):74–6.
19 Houry D, Feldhaus KM, Nyquist SR, Abbott J, Pons PT. Emergency Department Documentation in Cases of Intentional Assault. Ann Emerg Med. 1999;34(6):715–9.
20 Mc Closkey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate Partner Violence in Health Care Settings Leads to Women’s Receipt of Interventions and improved Health. Public Health Rep. 2006;121(4):435–44.
21 Fanslow JL, Norton RN, Spinola CG. Indicators of Assault- Related Injuries Among Women Presenting to the Emergency Department. Ann Emerg Med. 1998;32:341–8.
22 Abbott J. Injuries and illnesses of domestic violence. Ann Emerg Med. 1997;29(6):781–5.
23 Allen T, Noval SA, Bench LL. Patterns of injuries: accident or abuse. Violence Against Women. 2007;13(8):802–16.
24 Plattner T, Bolliger S, Zollinger U. Forensic assessment of survived strangulation. Forensic Sci Int. 2005;153 (2-3):202–7.
25 Fulton DR. Recognition and documentation of domestic violence in the clinical setting. Crit Care Nurs Q. 2000;23(2):26–34.
26 Houry D, Kaslow NJ, Kemball RS, McNutt LA, Cerulli C, Straus H, Rosenberg E, Lu C, Rhodes KV. Does screening in the emergency department hurt or help victims of intimate partner violence? Ann Emerg Med. 2008;51(4):433–42, 442.e1-7. Epub 2008 Mar 7
The authors declare no financial or commercial conflict of interest.