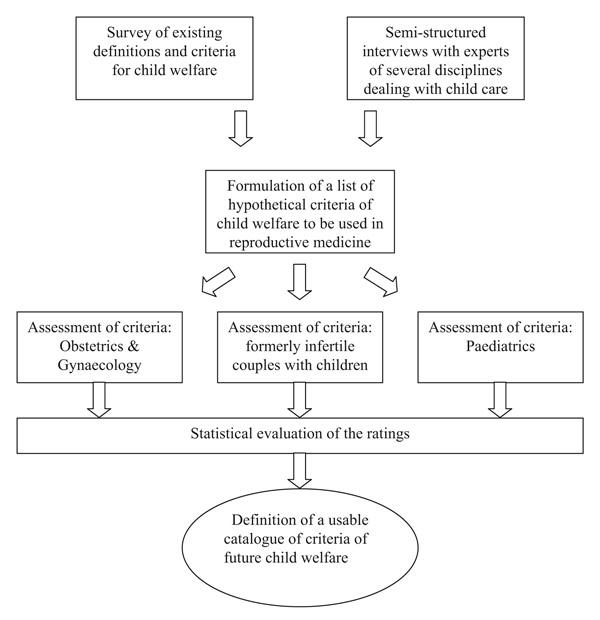
Figure 1
Design of the study.
DOI: https://doi.org/10.4414/smw.2010.13064
It is the vision of all physicians involved in assisted reproductive technology (ART) to support infertile couples in achieving a successful pregnancy and becoming parents of a healthy child. Oral contraception has paved the way for more self-determination and modern family planning, but this has also increased the trend towards delaying childbirth. With the ageing of both partners alike, the risk of infertility rises, which results in a steady increase in the demand for medical support to conceive a pregnancy. Over the years, modern reproductive technology has become increasingly effective and assisted reproductive medicine, in particular, now has the potential to overcome most causes of infertility.
In Switzerland, a comprehensive legislation was issued in 2001, which strictly regulates all aspects of assisted reproductive technology [1, 2]. This legislation stipulates that ART should only be used, when the future welfare of the child is foreseeable and secured (table 1). At first sight, this aspect of our legislation seems to fulfil the highest moral standards. However, in daily practice, physicians involved in infertility care are regularly confronted with the dilemma of deciding between their inclination to serve the woman’s desire for pregnancy and anticipated uncertainties concerning the child’s future welfare. Child welfare may be compromised in a physical sense by one of the most frequent complications of present-day reproductive medicine; multiple deliveries. Also, the future well-being of the child may be at risk socially in families living in a borderline socio-economic situation or psychologically when future parents are suffering from severe and long-lasting health problems.
Respecting the patient’s autonomy is a paramount principle of reproductive care tipping the physician’s decision in favour of treatment, but infertile couples may also seek assistance in treatment units with less stringent ethical considerations, for example outside Switzerland. Both obstetricians and paediatricians tend to criticise prior decisions of physicians involved in reproductive medicine, particularly when a pregnancy or delivery is burdened by complications bearing the potential to endanger the future health of the infant.
As a response to an ongoing debate at the University Hospital of Basel, Switzerland, we initiated a prospective study to assess the opinions of various stakeholders involved in the future welfare of children conceived with the support of assisted reproduction. For this purpose, we systematically searched the literature and screened a large array of existing definitions of child welfare, some issued by highly respected organisations, such as the WHO [3] and the UN’s Convention on the Rights of the Child [4], but also in use in various disciplines, such as human genetics, neonatology and family law. Based on a compilation of the available definitions and through complementary interviews with interdisciplinary professionals concerned with different aspects of child welfare, we formulated a list of hypothetical criteria for the future well-being of children. We then presented this list to members of three different stakeholder groups involved in various aspects of family care; notably physicians working in obstetrics and gynaecology, paediatrians as well as formerly infertile couples, now parents after successful assisted reproduction and experienced in raising their child(ren). Their assessments of each of the criteria were then compared and ranked based on their acceptance or rejection. The aim of this study was to evaluate differences and similarities in the opinions of the various parties involved in future welfare of the child in light of current legislation.
| Table 1Chapter 1, article 3 of the Swiss legislation on medically assisted reproductive medicine with regard to future child welfare [1]. |
| Assisted reproductive technology can only be applied when future child welfare can be guaranteed.They must be applied exclusively in couples,a. In whom parenthood is acknowledged.b. Who through their age and personal conditions are able to provide assistance and education to their child up to its adulthood.Donation of spermatozoa may only be performed in married couples.Gametes and oocytes in the pronucleate stage will not be used after the death of the person, from whom they arose. |
This study was carried out in four consecutive phases (fig. 1):
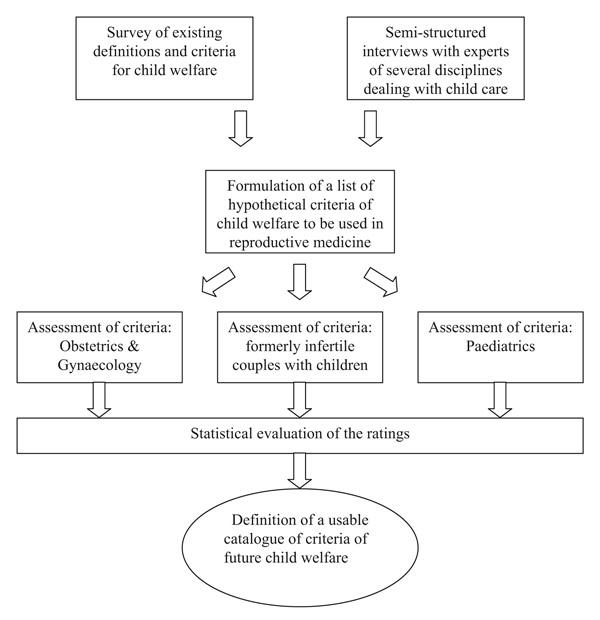
Figure 1
Design of the study.
1. Survey of existing definitions of child welfare formulated by various national and international organisations and institutions, followed by structured interviews with specialists of four different disciplines dealing with distinct aspects of child welfare, such as medical genetics, neonatology, family law and social workers involved in mediating adoption.
2. Formulation of 13 hypothetical criteria defining future child welfare, which could potentially be used for the assessment of the opinions of the various stakeholders.
3. Assessment of the formulated criteria by the three stakeholder groups involved in the care of mothers and/or their children, such as obstetrics and gynaecology and paediatrics, and formerly infertile couples, now parents after assisted reproduction.
4. Ranking of the hypothetical criteria based on the statistical assessment of ratings of each criterion and on the acceptance or rejection among the three groups.
Swiss legislation, regulating the use of assisted reproductive technology [1, 2], stipulates that future child well-being should be the first and exclusive motivating criterion for treatment. It also requests that both parents should be available for the child until it reaches adulthood (table 1). Other statements in the Swiss Code of Civil Law (ZGB) and Swiss Family Law were also taken into consideration [5, 6]. In addition, statements regarding child welfare in national legislation on assisted reproductive technology from the following countries were screened, such as Austria, Germany, France, United Kingdom, Belgium and Spain. Child welfare is defined in the articles 3, 9, 18, 21, 36 and 40 of the UN-convention (1989) [4], whereas the WHO focused on the health of the child as part of overall child welfare (1946) [3].
An extensive internet search was performed under the denominators “child” and “welfare” in the following databases: Google, PubMed, Bioethicsline, Psyndex.
After compilation of all the identified criteria and definitions of child welfare (table 2), a semi-structured interview plan was formulated and four semi-structured interviews were then held with experts representing distinct disciplines, each involved in different aspects of child welfare: medical genetics, neonatology, family law and social work for mediating adoption. The content of each interview was summarised by the second author (B.B.) and authorised by the experts.
All available material was processed stepwise following the methodology of Content Analysis [7]. Firstly, the entire bulk of information was reduced to central, meaningful content, then remaining questions and uncertainties were resolved by acquiring additional information, and, finally, the most important aspects of all information collected was structured down to essential messages. This process led to the formulation of 13 hypothetical criteria that could potentially be used for defining various aspects of future child welfare after ART (table 3). Each of these criteria was tagged with a Likert scale, with five possible assessments, ranging from “I do not agree at all” to “I fully agree”. These criteria were then given to 20 residents in obstetrics and gynaecology, to 21 residents in paediatrics, and were sent to 40 formerly infertile couples, whose youngest child was at least five years old and whose family planning was completed with the help of ART. The numbers of residents in obstetrics and gynaecology or paediatrics were chosen because of the number of qualified physicians available at that time in the respective departments. Before the questionnaire was given, our motivation for performing this study was explained within the frame of scientific presentations in the Children’s Hospital and the Women’s Hospital at the University of Basel, Switzerland. Each questionnaire sent to the parents (formerly infertile couples) was accompanied by a cover letter. The list of the hypothetical criteria, the accompanying letter to the couples and the design of the study were presented to and approved by the local ethics committee (EKBB 75/08).
Statistical evaluation of the assessments was carried out with Statgraphics Plus for Windows (Version 5.1, Manugistics Inc., Rockville, MD, USA) on a personal computer. The distributions of discrete data were analysed with non-parametric tests, such as Mann-Whitney U and Kruskal-Wallis. Statistical difference was set at the 5% level. The number of questionnaires was limited to the number of trained physicians available in the respective departments. As we assumed a broader variability in their opinions and a lower return rate of the questionnaires, we decided to send out 40 questionnaires to the couples. Due to the lack of published data related to the topic, no calculation of statistical power was performed.
| Table 2Sources for the 13 hypothetical criteria. | |
| Criterion | Source |
| Both parents’ life expectancy | Swiss Law on Assisted Reproduction [1,2] |
| Stable relationship between both partners [21] | |
| [22] | |
| [5] | |
| [23] pp. 1590–1591 | |
| Avoidance of future harm to the child | Convention on the Rights of the Child [4] |
| [23] | |
| Swiss Criteria for Adoption (Verordnung über die Adoptionsvermittlung, VAdoV) [6] | |
| Good prognosis of normal health of the child | Convention on the Rights of the Child [4]) |
| Swiss Law on Assisted Reproduction [1] | |
| Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference [3] | |
| Provision of education | Convention on the Rights of the Child [4] |
| Swiss Law on Assisted Reproduction [1] | |
| [23] | |
| [5] | |
| Shared home of both partners and the child | Convention on the Rights of the Child [4] |
| Swiss Law on Assisted Reproduction [1] | |
| Quality of the couple’s partnership | [23] |
| [21] | |
| [5] | |
| Social and financial living conditions | Swiss Criteria for Adoption (VAdoV) [6] |
| Adequate housing conditions | [6] |
| Swiss Law on Assisted Reproduction [1] | |
| Absence of mental illness in both partners | Swiss Criteria for Adoption (VAdoV) [6] |
| Swiss Law on Assisted Reproduction [1] | |
| Social network of the family | [6] |
| Limited age for paternal reproduction | experts’ opinion |
| Willingness for social integration | [6] |
| Table 3Description of the 13 hypothetical criteria, each defining a different aspect of future child welfare. |
| 1. Before the initiation of any infertility treatment the good health of both partners must be confirmed, so that both partners are capable of taking care of the child until its adulthood (both parents’ life expectancy until adulthood).2. Any treatment of infertility must be refused, when the rupture of the relationship between the partners is foreseeable (stable relationship between both partners).3. Any treatment of infertility must be refused, when one or both partners have been convicted of abuse, maltreatment or negligence, or when one or both partners have a history of violent behaviour (avoidance of future harm to the child).4. Any treatment of infertility must be refused, when due to hereditary or other disease, the risk (more than 25%) of mental of physical illness in the offspring is increased (good prognosis of normal health of the child).5. Any treatment of infertility must be refused, when it can be foreseen that the mental development of the offspring is endangered due to lacking provision of education in the society, in which it is supposed to be integrated (future provision of education to the child).6. Before initiation of any treatment of infertility the physician must ascertain that both partners will be available for their offspring. The physician must make sure that both partners envisage to continue their partnership and to live together until the adulthood of the child (shared home for both partners and their offspring).7. Any infertility treatment can only be provided to couples living together in a harmonious and loving partnership (good quality of the couple’s relationship).8. Any treatment of infertility can only be initiated, when the financial conditions of the couple have been verified and considered adequate to provide care to the child (adequate social and financial living conditions).9. The housing conditions of the infertile couple must be verified before initiation of any infertility treatment; the couple must declare that these conditions will be ascertained for a prolonged time period (adequate housing conditions).10. Any treatment of infertility should not be initiated when the mental condition of one or both partners is severely impaired. In the presence of any doubt, the mental health of both partners must be verified by an external physician (absence of mental illness in both partners).11. Any treatment of infertility can only be initiated, when the infertile couple is appropriately integrated in its social and cultural environment (sufficient social network of both parents).12. As age sets a biological limit to the time of reproduction in the female, the age limit for male reproduction must be set to 55 years, irrespective of the age of the female partner (limited paternal age for reproduction).13. An y treatment of infertility must be made dependent upon the willingness of both partners to integrate themselves into the society, in which the child grows up (willingness to integrate socially). |
The questionnaire included the 13 hypothetical criteria defining various aspects of future child welfare (table 3). They were sent to 40 couples and presented to 20 residents in obstetrics and gynaecology, and to 21 residents in paediatrics. The return rate among the physicians was 100%, and 25 out of 40 addressed former patients returned the questionnaires, which corresponds to a response rate of 62.5%.
Although all 13 hypothetical criteria were rated distinctively by the responding individuals, we could find no statistically significant differences in the distribution of the assessments among the three parties. Thereupon, we combined the assessments of each of the 13 criteria made by all parties and performed a ranking of the criteria, based on acceptance. For this purpose, we calculated the median values, the variance and the kurtosis of all assessments for each criterion (fig. 2). The criteria were then ranked according to a low median, a low variance and a high kurtosis.
The introduction of every new technology or protocol in ART has prompted systematic studies evaluating their safety, in particular with respect to avoiding harm to the offspring. Many notable examples can be brought forward to underline this effort, such as in the case of ICSI [8, 9], multiple births after ART [10], pre-implantation genetic diagnosis [11], use of ART in HIV patients [12] and both semen donation and motherhood surrogacy [13, 14], and ethical complications with pregnancy after ART have also been addressed [15]. In this regard, reproductive medicine has been at the forefront of an evidence-based approach in medicine. However, harm may be imposed through injudicious use of ART as well, as illustrated by spectacular cases such as the recent Californian octuplets, which have been discussed intensively in the serious lay press and beyond. This example and similar cases have repeatedly cast doubts on the judgment of some physicians involved in ART.
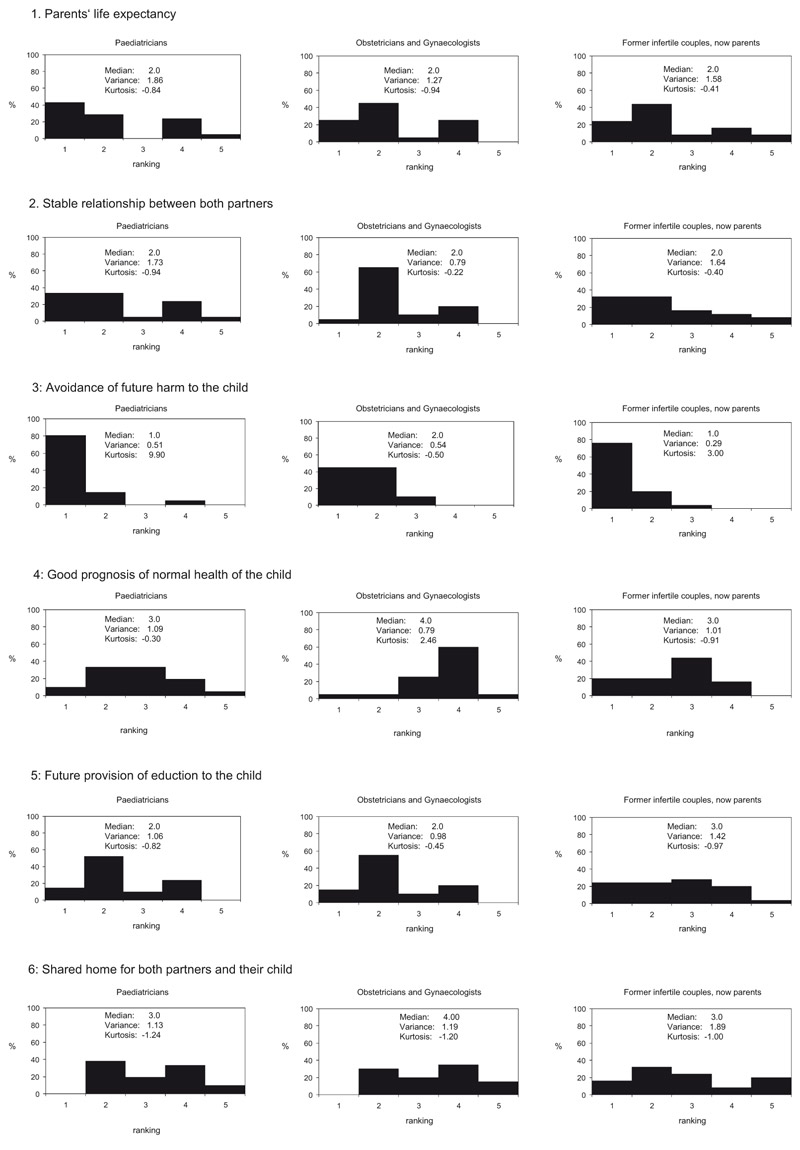
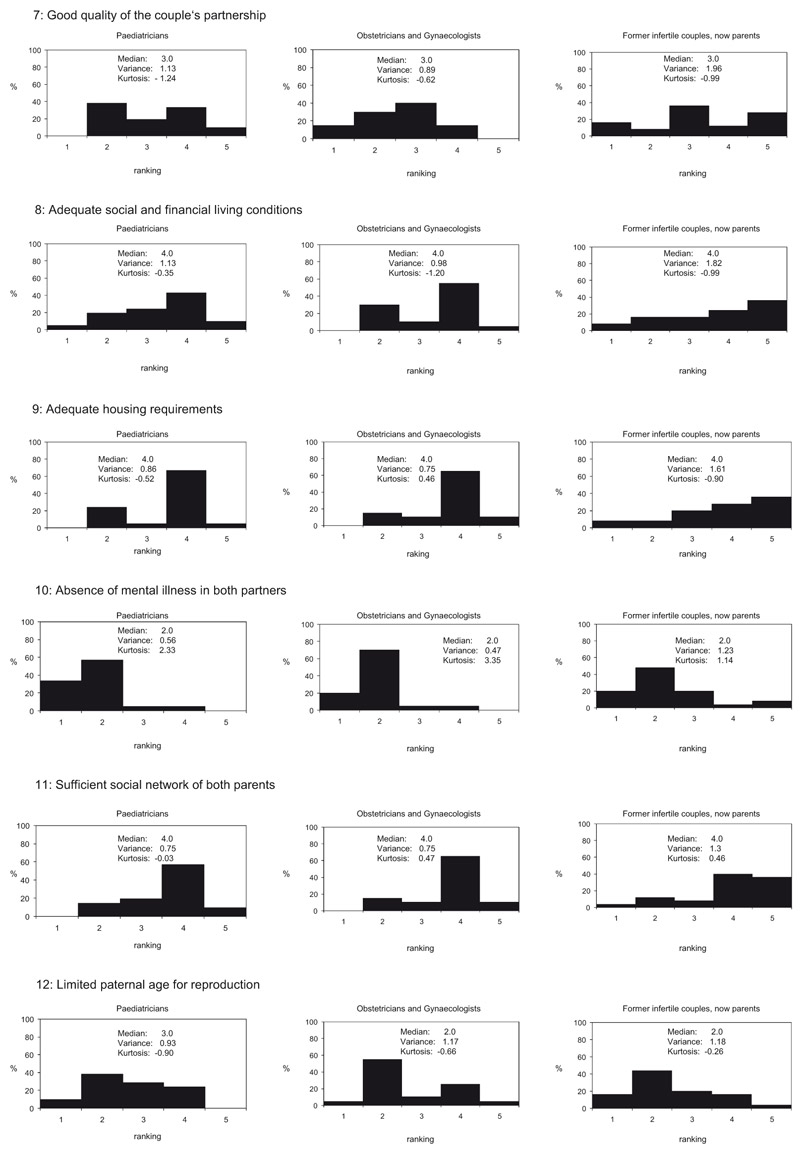
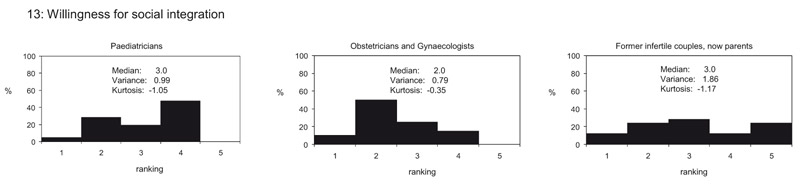
Figure 2
A, 2B and 2C: Distributions of the rankings given by paediatricians (n = 21), obstetricians and gynaecologists (n = 20), and former infertile patients, now parents (n = 25), to the 13 hypothetical criteria, previously elaborated based on definitions of child welfare formulated by various organisations, extracted from various legislations and given by principles in vigour in various disciplines. The distributions of the rankings given by the three assessing parties proved to be not significantly different, for all criteria
A restrictive legislation on the use of ART was issued in Switzerland in 2001, which stipulates that the future well-being of the child must rank as the most important criteria before initiating any treatment [2]. This specific restriction seems to be rather unique in legislation or codification about ART. The difficulties associated with such a “maximum level” threshold in the provision of medical care to infertile couples have been outlined previously [16]. This “maximum level” threshold contrasts with the “minimum level” threshold, which emphasises the autonomy of the couple and the avoidance of discriminating individuals living in a borderline socio-economic or health situation, whose right to procreation should be respected as well. The perception of clinicians who have to choose between these opposing ethical requirements has raised concerns among ethicists of the American Society of Reproductive Medicine (ASRM) [17]: on the one hand respecting the infertile couple’s autonomous choice (i.e. their wish for reproductive treatment) and, on the other hand, the need to prevent harm to a future child when the couple does not live in a favourable situation. This ongoing debate stresses the fact that the “maximum threshold” approach, as defined by Swiss Legislation, must be considered the least optimal.
In contrast, a Task Force on Ethics and Law of the European Society of Human Reproduction and Embryology (ESHRE) clearly states that the autonomy of the infertile couples is not absolute and they provide various recommendations to the physicians involved in order to ascertain the future welfare of the child, such as conditional treatment, referral to other organisations or refusal [18]. However, opinions among physicians may vary and this study was primarily motivated by apparent differences in the judgement of physicians involved in reproductive medicine on the one side and those involved in pregnancy and child care on the other. In order to examine the differences and similarities in the attitudes of various caretakers in pregnancy and neonatal care, we presented the list to three different parties for assessment, from whom we expected different rankings due to their distinct perspectives of child welfare. However, statistical examination of the returned questionnaires demonstrated that for none of the 13 criteria was the distribution of the rankings significantly different among the three evaluating groups. Obviously, even within each group, individuals came to entirely opposing conclusions during their assessments of each criterion. This result reflects the eminent difficulties of defining workable criteria for the prospective assessment of child well-being, as described before [16].
We then undertook a ranking of the 13 hypothetical criteria based on a statistical elaboration of the combined ratings, given by all members of the three assessing parties. A low median value of the distribution reflected the tendency towards accepting the criterion, whereas a high median value reflected the tendency towards rejecting it. A low variance was considered to reflect a low level of ambiguity, whereas a high kurtosis reflected a high level of agreement among the participants in their judgment. The ranking resulted from a stepwise assessment of first the median, then the variance and finally the kurtosis (table 4). From this analysis the following two criteria appeared as the most accepted: 1. “prevention of harm to the child”, and 2. “absence of mental illness in both partners”. The most rejected criteria were: 13. “acceptable social and financial conditions of living” and 12. “adequate housing conditions”. These criteria may have been rated lowest, either because these criteria were considered the least important, or because it is practically impossible to check whether they are being met by a couple, as was pointed out by some assessors in short footnotes.
The feedback from both the physicians and the couples, who rated the criteria “acceptable social and financial conditions of living” and “adequate housing conditions” as inappropriate, is in line with an ethical perspective focusing on social equity and fairness, especially regarding access to (reproductive) medicine. On the one hand, it would be hard to justify why couples with a less than average socio-economic position or accommodation should be denied medical assistance for becoming parents, when other couples living under similar circumstances can reproduce without comparable restraints. On the other hand, the anticipation of socio-economic difficulties for a future family should be perceived and appropriately addressed in a humane and wealthy society that can afford to apply sophisticated and costly technologies for treating infertility.
The assessments given by the three parties did not only converge regarding the rejection, but also the preference for the two positive criteria did: those accepted by the vast majority were “prevention of harm to the child” and “absence of mental illness in both partners”. It almost goes without saying that preventing harm is a paramount ethical principle [19], also traditionally inherent in the medical ethos and all its multiple codifications since the antiquities [20]. Yet, “harm” in its concrete form is to be prevented in the individual case. This is illustrated by the second preferred criterion: a parent with severe mental health problems may carry a serious challenge for the welfare of the whole family. Yet, where does “severe” begin? In a population with a life-time prevalence of depression reaching approximately 50%, we must distinguish carefully, in the name of fairness and against discrimination, between treatable and manageable mental disorders on the one side and those which are treatment-resistant and potentially disruptive.
It must also be noted that the only argument against the provision of treatment, as formulated in the Swiss legislation, “the liveliness and presence of both parents until the child reaches adulthood”, did not rank among the most accepted criteria in all three assessing groups.
One limitation of this study is that, although the questionnaires were supposed to be signed and dated by each participant, many responders, particularly the physicians, chose to anonymise their ratings. Therefore, the effect of the age and the gender of the assessors could not be examined. Another limitation of this study was the low number of questionnaires given to physicians, who were all working in a university hospital environment. A different profile of ratings might have been obtained among physicians working in a private practice, who may have a stronger inclination to embrace the needs of the infertile couples or future parents. This hypothesis could be tested in a further study.
Taking all the given statements together, the lack of differences in the assessments of most of the hypothetical criteria, among the three assessing groups, related more to the large variation in judgment among the various participants in each group, rather than to the intrinsic value of each of the criteria. This emphasises the difficulty in defining applicable criteria for child welfare and points out that we need a more differentiated approach at all levels of pregnancy care. The “maximum threshold” level for future childhood, which restricts medically assisted reproduction only to those couples that are able to guarantee future child welfare, is discriminating and is in conflict with the self-responsibility of many infertile individuals. Rather than being simply restrictive, all legal regulations should be directed towards an active management of those factors that have the potential to endanger future child welfare.
| Table 4Ranking of the 13 hypothetical criteria is based on the pooled assessments of the three parties. The criteria were ranked based on the returned questionnaires of 66 persons. The ranking was first based on the median value of the distribution, then on variance (below and above 1.0) and finally on kurtosis. | ||||
| Rank | Hypothetical criteria | median | variance | kurtosis |
| 1 | Avoidance of future harm to the child | 1 | 0.43 | 5.44 |
| 2 | Absence of mental illness in both partners | 2 | 0.81 | 4.14 |
| 3 | Limited paternal age for reproduction | 2 | 1.07 | –1.10 |
| 4 | Future provision of education to the child | 2 | 1.14 | 1.31 |
| 5 | Both parents’ life expectancy | 2 | 1.54 | –1.27 |
| 6 | Stable relationship between both partners | 2 | 2.36 | –0.94 |
| 7 | Good prognosis of normal health of the child | 3 | 1.12 | –1.09 |
| 8 | Willingness to integrate socially | 3 | 1.31 | –1.45 |
| 9 | Good quality of the couple’s relationship | 3 | 1.43 | –1.33 |
| 10 | Shared home for both partners and their child | 3 | 1.44 | –1.81 |
| 11 | Sufficient social network of both parents | 4 | 0.96 | 0.22 |
| 12 | Adequate housing conditions | 4 | 1.09 | –0.05 |
| 13 | Adequate social and financial living conditions | 4 | 1.33 | –1.37 |
We thank Prof. P. Miny, Prof. Ch. Bührer and Prof. U. Schaad, Children’s Hospital, and Prof. W. Holzgreve and Prof. J. Bitzer, Women’s Hospital, University of Basel, Switzerland, for their kind support of this study. We are also grateful to Prof. I. Schwenzer, Faculty of Law, University of Basel, and to Mrs. S. Oneta-Buholzer, Department of Education, Kanton Basel-Stadt.
1 Swiss Law on Assisted Reproduction, Bundesgesetz über die medizinisch unterstützte Fortpflanzung. Available from: http://www.admin.ch/ch/d/sr/8/810.11.de.pdf; 2001.
2 Germond M, Senn A. A law affecting medically assisted procreation is on the way in Switzerland. J Assist Reprod Genet. 1999;16:341-3.
3 Preamble to the Constitution of the World Health Organization (WHO) as adopted by the International Health Conference, New York, 1946.
4 Office of the UN High Commissioner for Human Rights. Convention on the Rights of the Child. Available from: http://www2.ohchr.org/english/law/crc.htm; 1989.
5 Honsel, H, Nedim PV, Geiser T. Basler Kommentar zum schweizerischen Privatrecht, Zivilgesetzbuch I: Art. 1 – 456 ZGB. Helbing & Lichtenhahn, Basel. Second edition. ISBN: 3-7190-2028-2; 2002.
6 Swiss Criteria for Adoption (Verordnung über die Adoptionsvermittlung, VAdoV). Available from: http://www.admin.ch/ch/d/sr/211_221_36/index.html; 2002.
7 Mayring P. Einführung in die Qualitative Sozialforschung. Beltz-Verlag, Hemsbach/Bergstrasse, Germany, fifth edition; 2009.
8 Leunens L, Celestin-Westreich S, Bonduelle M, Liebaers I, Ponjaert-Kristoffersen I. Cognitive and motor development of 8-year-old children born after ICSI compared to spontaneously conceived children. Hum Reprod. 2006;21:2922–9.
9 Belva F, Henriet S, Liebaers I, Van Steirteghem A, Celestin-Westreich S, Bonduelle M. Medical outcome of 8-year-old singleton ICSI children (born ≥32 weeks’ gestation) and a spontaneously conceived comparison group. Hum Reprod. 2007;22:506–15.
10 Bergh T, Ericson A, Hillensjö T, Nygren KG, Wennerholm UB. Deliveries and hildren born after in-vitro fertilisation in Sweden 1982-95: a retrospective cohort study. Lancet. 1999;354:1579–85.
11 Lavery S. Preimplantation genetic diagnosis and the welfare of the child. Hum Fertil. (Camb). 2004;7:295–300.
12 Tschudin S, Steimann S, Bitzer J, Hösli I, Holzgreve W, Elzi L, et al. Round-table multidisciplinary counselling of couples with HIV prior to assisted reproduction. Reprod Biomed Online. 2008;17:167–74.
13 Golombok S. New families, old values: considerations regarding the welfare of the child. Hum Reprod. 1998;13:2342–7.
14 Golombok S, Murray C, Jadva V, Lycett E, MacCallum F, Rust J. Non-genetic and non-gestational parenthood: consequences for parent-child relationships and the psychological well-being of mothers, fathers and children at age 3. Hum Reprod. 2006;21:1918–24.
15 Reiter-Theil S. Dealing with the normative dimension in clinical ethics consultation. Cambridge Quarterly Healthcare Ethics. 2009;8(4):347–56.
16 Pennings G. The welfare of the child. Measuring the welfare of the child: in search of the appropriate evaluation principle. Hum Reprod. 1999;14:1146–50.
17 The Ethics Committee of the American Society for Reproductive Medicine (2004) Child-rearing ability and the provision of fertility services. Fertil Steril. 2004;82:564–7.
18 ESHRE Task Force on Ethics and Law including Pennings G, de Wert G, Shenfield F, Cohen J, Tarlatzis B, Devroey P. (2007) ESHRE Task Force on Ethics and Law 13: the welfare of the child in medically assisted reproduction. Hum. Reprod. 2007;10:2585–88. –rearing ability and the provision of fertility services. Fertil Steril. 2004;82:564–7.
19 Beauchamp TL, Childress JF, editors. Principles of Medical Ethics. New York: Oxford University Press; 2001.
20 Troehler U, Reiter-Theil S, editors in collaboration with E Herych. Ethics Codes in Medicine: Foundations and Achievements 1947–1997. Ashgate, Aldershot; 1998.
21 Coester M. Das Kindeswohl als Rechtsbegriff. Die richterliche Entscheidung über die elterliche Sorge beim Zerfall der Familiengemeinschaft. Habilitationsschrift, Universität Augsburg; 114; 1983.
22 Sponsel R. Kindeswohl-Kriterien Deutschland. Internet Publicationen für Allgemeine und Integrative Psychotherapie. Available from: http://www.sgipt.org/forpsy/kw_krit0.htm; 2007.
23 Fegert J. Basic Needs of Children. In: Salgo L, Zenz G, Fegert J, Bauer A, Weber C, Zitelmann M, editors.Verfahrenspflegschaft für Kinder und Jugendliche. Ein Handbuch für die Praxis. Bundesanzeiger, Cologne, Germany. ISBN: 3-7190-2028-2; 2002.
This study was supported by the Repronatal Foundation in Basel, Switzerland.