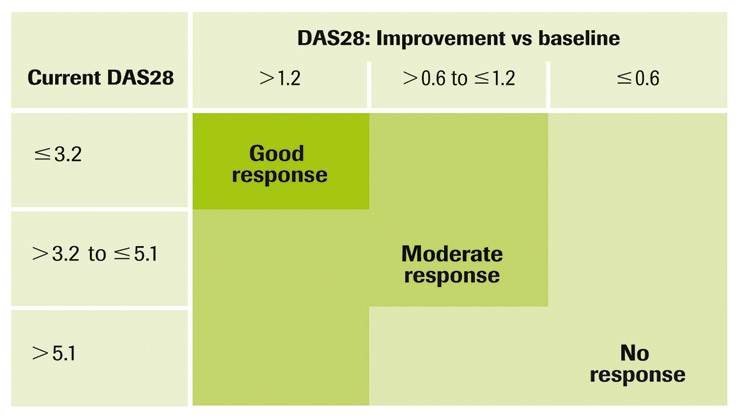
Figure 1
EULAR response criteria.
DOI: https://doi.org/10.4414/smw.2010.13073
Rituximab has been approved in Switzerland since 2006, in combination with methotrexate, for the treatment of moderate to severe active rheumatoid arthritis (RA) in patients with an inadequate response to anti-TNF therapies.
In clinical trials as well as in daily practice, rituximab has proven to be efficacious by improving clinical signs and symptoms as well as physical function and quality-of-life parameters [1–4]. In addition, 2 years’ X-ray data have clearly shown that rituximab reduces the rate of radiographic progression and inhibits joint damage [5, 6].
Finally, published data from clinical trials and follow-up studies confirm the good safety profile of rituximab, with data from more than 3000 patients with up to five treatment cycles not showing any increase in severe adverse events, infections or malignancies over time and/or with cycle number [7, 8].
Rituximab clearly differentiates itself from the other biological therapies for RA by its unique mode of action and unrivalled long dosing interval. While the long duration of response makes rituximab an attractive therapeutic option for RA patients, its effect decreases with time and re-therapy with rituximab is an essential part of a long term successful disease control.
Data from Switzerland, extracted from the SCQM-RA database, indicate a trend in the pattern of re-treatment with a shortening of the mean re-treatment interval from 11.9 months in 2006 to 9.4 and 7.8 months in 2007 and 2008 respectively [9]. However, optimal timing of re-treatment remains a matter of discussion.
Supporters of longer re-treatment intervals stress the higher convenience for patients, the lower costs and a potentially better safety, while supporters of early re-treatment and thus shorter and fixed re-treatment intervals emphasise improved and sustained efficacy.
The present document is intended to complement the international Consensus Statement on the use of rituximab in patients with RA published by Josef Smolen and his co-authors from the Working Group on the Rituximab Consensus Statement in 2007 [10], as there is a need for concise and usable guidelines regarding re-treatment with rituximab. Rheumatologists from the Swiss University Hospitals reviewed published data supporting different strategies of re-treatment and pooled their own experience and clinical practice in an effort to create such a consensus document specifically on rituximab re-treatment. The document is intended to improve and standardise the current practice in Switzerland using a pragmatic approach. This consensus is also endorsed by the clinical affairs group of the Swiss Society of Rheumatology (SSR/SGR) and the key principles on re-treatment will be incorporated into the SSR/SGR treatment guideline on rituximab. It can easily be assumed that any such recommendation is going to evolve over time as experience is gained and more information becomes available, e.g., on markers and predictors of response.
There is a large inter-individual variability in the duration of response to rituximab, a fact that makes it difficult to optimally time re-treatment. In principle there are two different options:
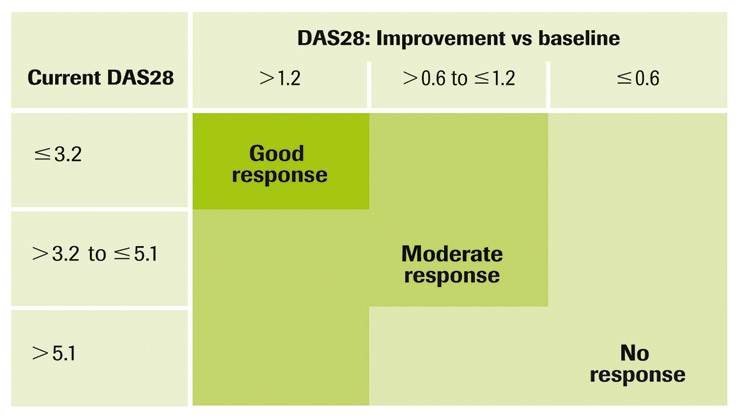
Figure 1
EULAR response criteria.
Individual re-treatment intervals, often referred to as “treatment on demand” and as recommended by Smolen et al. [10] are difficult to manage as no predictor of relapse is currently available. Too long intervals between two cycles of rituximab therapy imply the risk of relapses, a decrease of quality of life and potentially irreversible joint damage. The authors agreed that, in current practice, many patients still experience too large treatment intervals with evidence of flares at time of re-treatment [9].
Fixed and short re-treatment intervals would mitigate this risk of flare-ups and even potentially increase efficacy. However, fixed and short re-treatment intervals for all patients would decrease the convenience and cost saving of longer intervals, as well as potentially mitigate the capacity of the immune system to renew B-cells after repeated depletion. While concern about long-term safety is always legitimate, there is at present no data to substantiate a safety risk.
Data on re-treatment strategies remain scarce. More recent and post-launch clinical trials conducted by F. Hoffmann-La Roche AG and Genentech Ltd set out for fixed 6-month re-treatment intervals. A study specifically designed to check the effect of re-treatment on disease activity demonstrated that two courses of rituximab approximately 6 months apart resulted in improved and sustained efficacy at one year, as compared with a single course per year. Differences in efficacy between both groups were first observed following weeks 28 to 32, and patients receiving only one cycle per year had a two- to fourfold higher risk to loose their initial response (i.e., ACR 20 / 50 or 70). Furthermore, the safety profile of both study groups was comparable, in particular with respect to serious adverse events and severe infections [11].
When seeking to balance risk and benefit of different re-treatment strategies for the patient, multiple factors come into play, from treatment-related factors to patient-physician interaction-related factors. Clearly, the medication needs to be tailored to an individual’s need; this document aims to help the practitioner in his decision.
Disease activity and its evaluation remains a challenging concept. This recommendation uses the DAS28 index as a tool to simplify implementation of a standardised re-treatment strategy. DAS28 includes assessment of swollen and tender joints, pain and CRP or ESR. Its use allows defining the degree of disease activity as well as response to treatment (EULAR response criteria, fig. 1) [12]. However, the clinician should keep its limitations in mind, and individual components of the DAS28 as well as other symptoms of disease activity such as fatigue have also to be evaluated for concordance with the DAS28 value and the EULAR response.
The authors further advocate yearly x-rays of hands and feet to evaluate radiological progression. However, radiological data is not considered to prevail over disease activity. Hence treatment should not be pursued in the absence of clinical response.
Finally, determination of anti-CCP and rheumatoid factor (RF) is certainly most useful before starting rituximab therapy, as higher probability of response is obtained in seropositive patients [13]. However, there is no unequivocal evidence that repeated testing of auto-antibodies will help to optimise re-treatment.
Rituximab usually leads to rapid B-cell depletion. There is also a certain association between loss of response and return of B cells [14], but analytical techniques need to be refined and further validated before any monitoring of B cells or other parameters can be broadly applied for scheduling re-treatment in individual patients.
Persistent or re-emerging inflammatory activity in the synovium can be displayed by joint B-mode ultrasound [15] and the use of ultrasound may also be helpful in difficult cases to decide on re-treatment. However, as for B cell markers, its role in clinical practice needs to be further defined by studies and confirmed by validation for this specific purpose.
Despite recent publications regarding a new case of PML in an RA patient treated with rituximab [16], the authors believe that, considering the rarity of the cases and the lack of causal relationship with repeated courses of rituximab, the present recommendation remains valid until further data become available, in particular in an TNF-inadequate responders’ population. However, physicians should consider this diagnosis in the presence of neurological symptoms.
Considerations regarding re-treatment depend on the observed response to rituximab treatment which can be categorised into 3 different outcomes based on DAS28 and EULAR response rates:
1. no response or no significant response
2. definite response with significant residual disease activity
3. definite response with low or minimal disease activity
The authors recommend that response to rituximab treatment be evaluated between 3 to 4 months after the initial infusion. After this time point it becomes unlikely that patients with no response will experience a significant decrease in disease activity. These patients should therefore be managed further as outlined below for “non-responders”.
For patients with definite response at 3 to 4 months, the degree of response should be re-evaluated at a further time point around 6 months, when decision about re-treatment is going to be taken according to the above response categories.
Re-treatment strategy differs for the 3 above mentioned categories of initial response to rituximab as summarised in table 1 and as further explained below:
These patients do not show any significant change in disease activity upon the first rituximab treatment (non-response as defined by the EULAR criteria, fig. 1).
There is no objective evidence to support that these patients should receive an additional course of rituximab if therapeutic alternatives are available [17].
For the rare patient with no alternatives, it could be reasonable to envisage a second course of rituximab, some data having shown occasional benefit of re-treatment in this non-responder population [18].
These patients experience a distinct response to rituximab, usually described as moderate response according to EULAR criteria. However, they did not achieve low or minimal disease activity at the 6-month time point. These patients have persistent disease activity that will lead to progressive joint destruction and disability.
In accordance with the prevailing treatment paradigm in RA [19, 20] according to which remission is the aim, these patients’ treatment should be optimised without delay and re-treatment used to further lower disease activity and avoid flares. These patients should be re-treated at the earliest studied time point, which is around 6 months after the previous cycle of rituximab.
Published data have shown that repeated courses of rituximab increase the efficacy relative to original baseline and were well tolerated [3, 4, 21]. In rituximab responders, two courses of rituximab approximately 6 months apart resulted in a significantly improved efficacy at one year as compared with a single course within the same year, and this with a comparable safety profile [11]. Furthermore, the latest evaluation of SCQM-RA data confirms that the mean disease activity starts to rise again 6 months after a treatment course [9, 22].
As the effect of rituximab re-treatment is not immediate and needs approximately 2 months to fully develop, there is no reason to delay re-treatment beyond 6 months as this patient group still has active disease. Finally, as remission should be achieved as fast as possible, adequate use of concomitant DMARD or glucocorticoid treatment (e.g., intra-articular or bridging glucocorticoids) should be considered, as well as alternative biologic treatment strategies if the desired treatment success has not been reached with repeated courses.
These patients experienced a major response with low or minimal residual disease activity following a treatment cycle of two infusions of rituximab, which pragmatically is best described as a DAS28 <3.2 or even <2.6. To qualify for this patient category, a response should already be obvious at 3 to 4 months after treatment and should be maintained or improved at 6 months.
In this category, optimal timing of re-treatment remains a matter of discussion between the advocates of longer intervals and those in favour of shorter and fixed re-treatment intervals. The majority of the authors of this document would rather adopt a “wait and see” strategy, accepting some gap of optimal disease control against the potential harm due to multiple repeated courses, while the minority would favour a fixed 6-months re-treatment protocol for this patient category as well or at least a very aggressive “wait and see” strategy in the hope to optimise efficacy over risks.
In any case, but in particular with a “wait and see” strategy, regular monitoring visits are mandatory to detect signs of disease flare-up. The rheumatologist should check for swollen and tender joints, and other clinical signs and symptoms or lab parameters (ESR or CRP) that would indicate disease reactivation. Additionally, the patient should be thoroughly educated to contact his physician as soon as the first symptom of flare-up arises. For a well-educated patient, quarterly visits may be appropriate; else, more regular visits should be planned.
An increase in DAS28 as well as any other sign of disease activity should trigger re-treatment. A prompt re-treatment of any patient experiencing even mild symptoms of increasing disease activity would provide the best chance to remain in low disease activity state or remission. Only a very minor proportion of patients will remain in rituximab-induced remission for more than one year. The authors feel that re-treatment usually should not be delayed beyond one year with annual x-rays to make sure that the disease is not erosive despite low disease activity. Any observation of progressive joint damage or inflammatory activity in the synovium would deserve a more aggressive approach.
Until further data become available, the authors recommend a dosage of 2×1000 mg for re-treatment as approved by the health authorities, especially as the use of 2×500 mg per cycle did not seem to demonstrate a similar benefit on structural damage in the ongoing IMAGE study [23].
| Table 1Summary of re-treatment algorithms based on initial response criteria. | |||
| Category of response | Criteria of response | Timing of re-treatment | Actions / Remarks |
| Non-responders | – DAS28 improvement <0.6– No moderate EULAR response | – No RTX re-treatmentif therapeutic alternatives are available.– RTX re-treatment can be considered in the absence of reasonable alternatives | Stop treatment if no response after second cycle |
| Responders with residual disease activity | – DAS28 improvement >0.6– Residual DAS28 ≥3.2– Moderate EULAR response | – Re-treat at 6 months,aiming for optimal response | – Re-evaluate after re-treatment, if still with residual activity, consider alternatives biological |
| Optimal responders in remission or with low disease activity | – DAS28 <2.6 or <3.2 | – “Wait and see” – Re-treat at any sign of returning disease activity: not earlier than after 6 months | – Educate patient– Physician sees patient at least quarterly to check joints and inflammation parameters– Do not delay re-treatment until full flare-up |
Rituximab has proven to be efficacious in the treatment of RA. Despite its long duration of response, re-treatment remains an essential part of a successful therapy. In practice, many patients on rituximab experience flare-ups as treatment intervals are too long. Optimal treatment intervals remain a matter of discussion. This document aims to improve and standardise the current practice in Switzerland using a pragmatic approach. It is suggested that disease evaluation be based on DAS28 and EULAR response criteria while also considering quality of life criteria and radiographic progression. Three categories of response have been defined requiring a different strategy of re-treatment
1. Non-responder patients not achieving at least moderate EULAR response would not receive rituximab re-treatment if other therapeutic options are available.
2. Responders with remaining residual disease activity should generally be retreated after 6 months to maintain and improve response.
3. Patients achieving low or minimal disease activity are considered optimal responders. The majority of the authors recommend a “wait and see” strategy with treatment intervals that rarely exceed 12 months. Patients should be trained to see the doctor upon first signs of relapse. Erosive disease should be treated more aggressively to avoid irreversible joint damage.
Optimisation of re-treatment means balancing risk and benefit for the patient and some rheumatologists will favor a more cautious approach than others. Tailoring of individual treatments is necessary, and this document aims to help the practitioner in this difficult decision until markers and predictors of response and relapse become available.
1 Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC, et al. Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: Results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum. 2006;54(9):2793–806.
2 Keystone E, Burmester GR, Furie R, Loveless JE, Emery P, Kremer J, et al. Improvement in patient-reported outcomes in a rituximab trial in patients with severe rheumatoid arthritis refractory to anti-tumor necrosis factor therapy. Arthritis Rheum. 2008;59(6):785–93.
3 Keystone E, Fleischmann R, Emery P, Furst DE, van Vollenhoven R, Bathon J, et al. Safety and efficacy of additional courses of rituximab in patients with active rheumatoid arthritis: an open-label extension analysis. Arthritis Rheum. 2007;56(12):3896–908.
4 Keystone EC. Efficacy and safety of repeat treatment courses of rituximab in RA patients with inadequate response to Tumor Necrosis Factor inhibitors: Long-term experience from the REFLEX study [abstract]. Arthritis Rheum. 2008.
5 Cohen S, E.C. K, Genovese MC, Emery P, Peterfy C, Tak PP, et al. Continued inhibition of structural damage in rheumatoid arthritis patients treated with rituximab at 2 years: REFLEX study (abstract). Ann Rheum Dis. 2008;67(Suppl II):189.
6 Keystone E, Emery P, Peterfy CG, Tak PP, Cohen S, Genovese MC, et al. Rituximab inhibits structural joint damage in patients with rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitor therapies. Ann Rheum Dis. 2009;68(2):216–21.
7 Van Vollenhoven FR, Emery P, Bingham III CO, Keystone EC, Fleishmann RM, Furst DE, et al. Long-term safety of patients receiving rituximab in rheumatoid arthritis clinical trials. J Rheumatol. 2010;37(3):558–67.
8 van Vollenhoven RF, Emery P, Bingham III CO, Keystone EC, Fleishmann RM, Furst DE, et al. Long-Term Safety of Rituximab: Long-Term Follow-up of the RA Clinical Trials and Retreatment Population [abstract]. Arthritis Rheum. 2009;60(Suppl 10):1952. DOI: 10.002/art.27025.
9 Finckh A, Courvoisier D, Ciurea A, Brulhart L, Kyburz D, Scherer A, et al. Longterm treatment with RTX in RA: evidence for a learning curve by rheumatologists [abstract]. Ann Rheum Dis. 2009;68 (Suppl 3):438.
10 Smolen JS, Keystone EC, Emery P, Breedveld FC, Betteridge N, Burmester GR, et al. Consensus statement on the use of rituximab in patients with rheumatoid arthritis. Ann Rheum Dis. 2007;66(2):143–50.
11 Mease PJ, Cohen S, Gaylis NB, Chubick A, Kaell AT, Greenwald M, et al. Efficacy and safety of retreatment in patients with rheumatoid arthritis with previous inadequate response to tumor necrosis factor inhibitors: results from the SUNRISE trial. J Rheumatol. 2010;37(5):917–27.
12 Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis. 2009;68(6):954–60.
13 Isaacs JD, Olech E, Tak PP, Deodhar A, Keystone E, Emery P, et al. Autoantibody-positive RA patients have enhanced clinical response to RTX when compared with seronegative patients [abstract]. Ann Rheum Dis. 2009;68(Suppl 3):442.
14 Moller B, Aeberli D, Eggli S, Fuhrer M, Vajtai I, Vogelin E, et al. Class-switched B cells display response to therapeutic B-cell depletion in rheumatoid arthritis. Arthritis Res Ther. 2009;11(3):R62.
15 Ziswiler HR, Aeberli D, Villiger PM, Moller B. High-resolution ultrasound confirms reduced synovial hyperplasia following rituximab treatment in rheumatoid arthritis. Rheumatology. (Oxford). 2009;48(8):939–43.
16 Fleischman RM. Progressive multifocal leukoencephalopathy following rituximab treatment in a patient with rheumatoid arthritis. Arthritis Rheum. 2009;60(11):3225–28.
17 Thurlings RM, Vos K, Gerlag DM, Tak PP. Disease activity-guided rituximab therapy in rheumatoid arthritis: the effects of re-treatment in initial nonresponders versus initial responders. Arthritis Rheum. 2008;58(12):3657–64.
18 Vital EM, Dass S, Rawstron AC, Buch MH, Goeb V, Horner EA, et al. Management of non-response to rituximab in rheumatoid arthritis: predictors and outcome of retreatment. Arthritis Rheum. 2010;doi 10.1002/art.27359.
19 Bykerk V. Unmet needs in rheumatoid arthritis. J Rheumatol Suppl. 2009;82:42–6.
20 Drossaers-Bakker KW, de Buck M, van Zeben D, Zwinderman AH, Breedveld FC, Hazes JM. Long-term course and outcome of functional capacity in rheumatoid arthritis: the effect of disease activity and radiologic damage over time. Arthritis Rheum. 1999;42(9):1854–60.
21 Keystone EC, Fleischmann R, Emery P, Dougados M, Baldassare AR, Armstrong GK, et al. Multiple Courses of Rituximab (RTX) Produce Sustained Efficacy in Patients (pts) with Rheumatoid Arthritis (RA) with An Inadequate Response (IR) to One or More TNF Inhibitors [abstract]. Arthritis Rheum. 2009;60(Suppl 10):1683. DOI: 10.002/art.26757.
22 Finckh A, Ciurea A, Brulhart L, Moller B, Walker UA, Courvoisier D, et al. Which subgroup of rheumatoid arthritis patients benefits from switching to rituximab versus alternative anti-TNF agents after previous failure to anti-TNF agent? Ann Rheum Dis. 2010;69(2):387–393.
23 Tak PP, Rigby WF, Rubbert-Roth A, Peterfy CG, van Vollenhoven RF, Stohl W, et al. RTX in combination with MTX significantly inhibits joint damage and improves clinical outcomes in patients with early active RA who are naïve to MTX (IMAGE) [abstract]. Arthritis Rheum. 2009;60(Suppl 10):636 DOI: 10.1002/art.25716.
The cost of the meetings necessary for this work have been supported by Roche AG. Dr ing Ute Schmiedel works for Roche AG.