Physiotherapy-mediated physical activity and patient education: active agents with great effect and hardly any side effects
In 2019, around 2.41 billion people worldwide were affected by noncommunicable diseases, with musculoskeletal disorders being the predominant condition with respect to lived years with disability (YLD). Musculoskeletal disorders have contributed to a cumulative total of 310 million YLD, and most of these cases could potentially have been improved with medical assistance at some stage. Globally, the number of noncommunicable disease cases increased by 63% from 1990 to 2019. In the same period, a similar situation was observed in Switzerland, where 3.9 million people experienced noncommunicable diseases, for a total of 500,000 YLD (figure 1). Also in Switzerland, musculoskeletal disorders emerged as the leading cause of disability, with low back pain and osteoarthritis being the primary contributing conditions. Concurrently with this increase in noncommunicable diseases, we face a decrease in the number of primary care physicians actively working in the Swiss cantons, who are expected to play a key role in prescribing cost-effective treatments. This development places considerable strain on the healthcare system. How can we surmount this challenge?
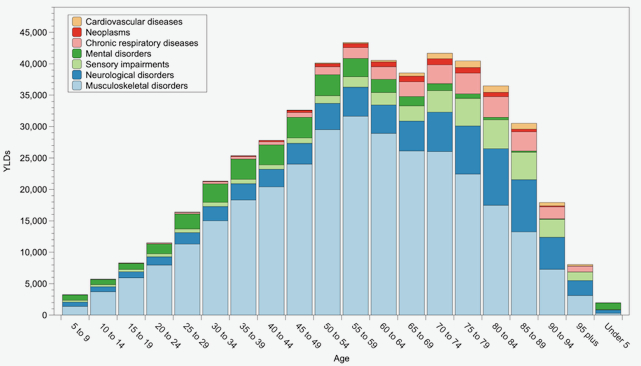
Figure 1. Years lived with disabilities (YLD) for Switzerland for selected conditions (Institute for Health Metrics and Evaluation (IHME). WHO Rehabilitation Need Estimator. From: https://vizhub.healthdata.org/rehabilitation/).
Current healthcare processes and infrastructures focus on curative care in acute care hospitals and, in some cases, on inpatient rehabilitation. Common treatment options include surgical and pharmacological interventions. Those allow patients to remain passive while they are treated, aligning with the common expectation of receiving care without active personal involvement. However, it has become increasingly evident that the current healthcare system is not sufficient for managing the growing demand which is largely related to the rising number of people with noncommunicable diseases.
Nevertheless, other effective evidence-based treatment options are currently only represented to a small extent in the Swiss healthcare system and are accordingly underutilized. Among those, physical activity, including targeted exercise, offers substantial potential. Physical activity is defined as any bodily movement produced by skeletal muscles that requires energy expenditure. Exercise, on the other hand, is a subcategory of physical activity that is planned, structured, and purposefully focused on improvement or maintenance of one or more components of physical fitness. It has been shown that physical activity is very effective in secondary prevention through exercise treatments of noncommunicable diseases, while also being a very low-risk intervention. Unlike a pill, however, physical activity cannot be swallowed. It is a strenuous intervention in which much of the responsibility lies with those involved, and it can only be effective if individuals develop self-efficacy. As physical activity is also inexpensive, the economic incentives are smaller, which could be a reason for its poor implementation. In countries outside of Switzerland, targeted exercise is already a well-established component of the health service. After seeing a doctor, patients may leave the practice with an exercise prescription, as exercise is considered a therapeutic measure. “Exercise is medicine” even became a global health initiative with 40 member countries. Even if the evidence for the effectiveness of exercise is clear and overwhelming, in Switzerland the first-line management of patients with osteoarthritis often still consists of a wait-and-see approach, in some cases in combination with symptom-relieving medication. For example, for osteoarthritis of the knee, a meta-analysis of 42 studies, or almost 7000 patients, concluded that no further studies are needed to confirm the effectiveness of exercise in terms of pain relief compared to no or minimal treatment. There are also initiatives to close this gap between evidence and current practice, for example the program Good Life with Osteoarthritis in Denmark (GLAD) from the University of Southern Denmark. It was originally developed and introduced in Denmark in 2013 and has been adopted by other countries, among them Switzerland. At the end of 2022 the Swiss GLAD register had longitudinal data of approximately 2500 participants. The analyses confirmed the effectiveness of the exercise and patient education approach. This program is only one example. There are several additional areas where physical activity combined with patient education has proven to be effective, such as the Diafit program for patients with pathological glucose tolerance and physical activity promotion for patients with cancer.
Driven by societal changes, physiotherapists are expected to become experts in coaching patients in self-management and behaviour change, using physical activity as a means. In Switzerland, professional training of physiotherapists moved to universities of applied sciences in 2006, and physiotherapy has moved from a profession of predominantly executing professionals who received prescribed interventions, towards an academic profession. An academic profession is characterized in part by the fact that its education is at a tertiary level, and it develops its activities according to scientific criteria. Many physiotherapists now possess scientific training at the bachelor's, master's, or even doctoral level. Driven by research conducted by physiotherapists, physiotherapy has developed effective, appropriate, and economical interventions, frequently incorporating targeted exercise combined with patient education.
Noncommunicable diseases are characterised by a fluctuating course, with exacerbations and quiet phases. It is debateable whether those patients always need to see a GP when health-related issues arise. Alternatively, it is conceivable that other healthcare professionals might get involved with managing these patients. This would for example mean that patients with chronic musculoskeletal conditions see a PT instead of a GP – so-called direct access that would be new for Switzerland. A recent systematic review investigated the effectiveness and consequences of direct access. The 28 included studies reported on direct access for over 32000 patients with musculoskeletal disorders. The authors concluded that direct access to physiotherapy, in comparison with the physician-led model, is safe and equally effective concerning health outcomes. Another conclusion was that the medical model saw a greater use of imaging, drug prescribing, and referrals to another specialist. Consequently, direct access to physiotherapy was found to be more cost-effective.
In conclusion, this article explains the paradigm shift in physiotherapy that began with academization in 2006 and is still ongoing based on demographic changes. The above examples illustrate how physiotherapy interventions are playing a greater role in the management of noncommunicable diseases and are increasingly based on sound scientific evidence, which highlights the contribution that physiotherapists can make to the prevention and treatment of noncommunicable diseases. With its evidence-based approaches, physiotherapy is helping the Swiss healthcare system to overcome some of its challenges.
Lara Allet, Haute école spécialisée de Suisse occidentale Valais-Wallis - Haute Ecole de Santé, Sion, Switzerland; lara.allet[at]hevs.ch
Marco Barbero, University of Applied Sciences and Arts of Southern Switzerland, Department of Business Economics Health and Social Care, Rehabilitation Research Laboratory 2rLab, Manno, Switzerland; marco.barbero[at]supsi.ch
Heiner Baur, Berner Fachhochschule, Department Gesundheit, Fachbereich Physiotherapie, Bern, Switzerland; heiner.baur[at]bfh.ch
Eling D. de Bruin, ETH Zürich, Institut für Bewegungswissenschaften und Sport, Zürich, Switzerland, and Ostschweizer Fachhochschule, St. Gallen, Switzerland; eling.debruin[at]hest.ethz.ch
Markus Wirz, ZHAW Zürcher Hochschule für Angewandte Wissenschaften, Institut für Physiotherapie, Winterthur, Switzerland; markus.wirz[at]zhaw.ch
